Pelvic Floor Exercises For Men And Women
In addition to the training with the probes, you can train your pelvic floor with special exercises.
Pelvic floor exercise for men: The wall runner
Lie on your back for the exercise and place your feet at right angles to the wall. Breathe out and lift the pelvis so that it no longer touches the floor. While inhaling, lower the pelvis again until just before the floor. If you want to increase the level of difficulty, you can lift the pelvis, hold this position and run up and down the wall with your feet.
You can repeat this exercise 5 – 10 times a week.
Pelvic floor exercise for women: The Hump
For this exercise you will go into the quadruped position. The hands are shoulder-width apart and the wrists form a line with the shoulder joints. Breathe in and change your back position into a slight hollow back. When you exhale, make a cat hump and tense your pelvic floor muscles.
You can repeat the exercise 15 – 20 times a week.
Here you will find more pelvic floor exercises for women and pelvic floor exercises for men.
Nerve Stimulation To Treat Urinary Incontinence
Topics in this Post
Many people have heard of pacemakers and how they can be used to treat heart conditions. But did you know a similar implantable device is available to treat urinary incontinence?
Urinary incontinence, or the loss of bladder control, is common. One of the most common types is urge incontinence, which is distinguished by a sudden, intense urge to urinate followed by an involuntary loss of urine. About 17% of women and 3% to 11% of men experience urge incontinence at some point in their lives.
Symptoms of incontinence can cause people to feel socially isolated, experience sexual inhibition, or become afraid to make social or travel plans. Careers and personal relationships are often affected.
Fortunately, many treatment options can help, including sacral neuromodulation.
Muscle Stimulation For Strength Control Stability And Performance
If you have read this far you will realize that the pelvic floor has an extensive array of muscles and connective tissues, and is richly endowed with blood vessels and nerves, making it highly responsive to assisted exercise using electrical stimulation.
It is also important to remember that the bladder detrusor and the internal sphincters are all smooth or involuntary muscle and cannot respond to manual exercise. Electrical stimulation is the only external way to stimulate the nerve fibres supplying these muscles.
The perineum anatomy determines the best location for electrode placement for all of the above applications – incontinence, support, stability and sexual performance.
It is not desirable or necessary to stimulate the muscles directly. Rather, the objective is to stimulate the motor nerves and sympathetic nerve fibres that supply the relevant muscles, i.e. the various branches of the pudendal nerve, the ventral primary rami and the parasympathetic fibres.
Our recommendation is to:
-
One large electrode over the sacrum, i.e. the large, triangular bone at the base of the spine and above the coccyx
The area between the pads is large enough to cover and stimulate all the motor nerves and sympathetic nerve fibres in question.
Dose is determined by intensity, the number of muscle contractions per day and the number of days in the program of treatment.
Recommended Reading: Dx Code For Urinary Frequency
Incontinence Is The Silent Disabler
You are not alone – approximately 5 million Australian men and women experience some degree of incontinence, and almost all are suffering in silence.
It is both easy and wise to address the issue as soon as it manifests itself. If you don’t tackle the problem soon:
-
It will not get better on its own – wishful thinking does not work
-
It will get worse as you age
-
Eventually, you will be mopping up the symptoms
-
YES, the purchase and wearing of incontinence pants or pads
-
This is expensive, uncomfortable, inconvenient and potentially embarrassing
-
For the rest of your life!
And there is another major concern to mention. There is:
-
A proven link between incontinence and urinary tract infection
-
A proven link between UTI in the elderly and fever induced delirium
-
A proven link between delirium and dementia
Why is no-one talking about this?
-
Physiotherapists know that weak pelvic floor muscles are a major cause of incontinence
-
Primary care doctors know that untreated incontinence is a cause of UTI
-
Geriatricians know that chronic UTI’s in the elderly are a cause of delirium
-
Neurologists know that delirium exacerbates dementia
Who is joining the dots?
Percutaneous Tibial Nerve Stimulation
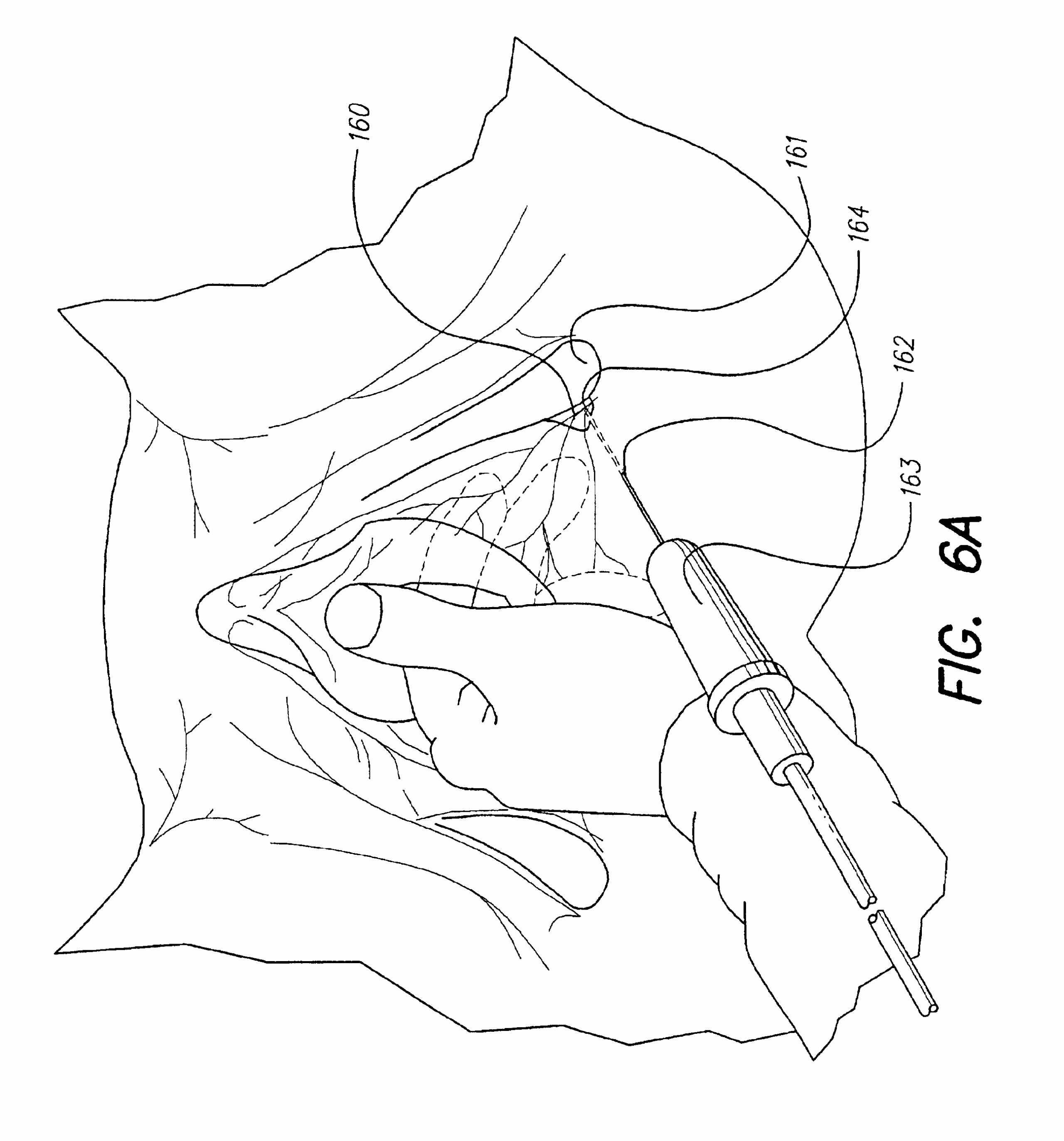
A female patient is using Percutaneous Tibial Nerve Stimulation to help control her urinary incontinence. An electrode is placed only at the ankle area.
Percutaneous Tibial Nerve Stimuation is a low-risk, non-surgical treatment. PTNS works by indirectly providing electrical stimulation to the nerves responsible for bladder and pelvic floor function. During PTNS treatment, the patients foot is comfortably elevated and supported. Also during treatment, a slim needle electrode is placed near the nerve at the ankle known as the tibial nerve. A device known as the Urgent PC Stimulator is connected to the electrode and sends mild electrical pulses to the tibial nerve. These impulses travel to the sacral nerve plexus, the group of nerves at the base of the spine responsible for bladder function.
PTNS is a form of electroacupuncture. You can find out more about this by reading our information on acupuncture.
Who Can Benefit from PTNS Treatment?
This therapeutic treatment is for patients experiencing overactive bladder symptoms of urinary urgency, urinary frequency and/or urge incontinence. PTNS has been approved by regulatory agencies outside the United States to treat fecal incontinence, but has not been approved for this usage in the US at this time. PTNS is generally used after behavior modifications, Kegel exercises and failure of medications.
Who Cannot Use Percutaneous Tibial Nerve Stimulation
Positive Aspects of Percutaneous Tibial Nerve Stimulation
Things to Remember
Read Also: Urinary Tract Infection And Incontinence
A Stimulation Current Treatment Is Targeted And Gentle For Incontinence
Incontinence occurs in both men and women and can start from the age of 20, as from this point our muscle mass tends to decrease. If one loses control of the bladder or bowel, those affected suffer from fear and shame and avoid talking about it. Very often incontinence is caused by too weak pelvic floor muscles, which are responsible for the function of the bladder and bowel sphincter muscles. Electro-stimulation can be used to strengthen the muscles of the pelvic floor.
How Should We Use Tens
We now think that it can be effective using it 2 to 3 times a week for at least a 6 week period. If used in conjunction with exercise and bladder training, it may help the other interventions to work better.
We have always known that the electrodes could be placed on the sacrum . We have also known in more recent years that the electrodes could be placed at the inside of the ankle. This is where a particular nerve is very close to the skin: it is called the posterior tibial nerve and it exits the sacrum at the same level as the nerves to the bladder.
Also Check: Can Urinary Incontinence Cause Uti
Why Is Ankle Superior
We now know that we can set the parameters of the TENS, ie the intensity and the frequency of the impulses, by actually looking for a small muscle twitch of the toe. Once we find this, we know the TENS is in the correct place making it more accurate. With the sacrum placement, we have no sign to show us we are getting to the right nerves. So we now know that the ankle placement is the better option.
The following picture shows the approximate placing of the electrodes at the ankle:
If you would like help with overactive bladder or feel frustrated that other approaches havent helped, come and see us. We can sell the TENS to you for around $60 . Or we can help you source one online. They can become quite costly with added features so be careful: for this treatment a simple TENS like the one shown above is fine.
Improving Urinary Incontinence With Electrical Stimulation And Exercise
Patient Information: Female, Age 74
Diagnosis: Urinary Incontinence / Hip Fracture
History:This woman was admitted to a skilled nursing facility with significant decline in mobilityand function after an extended hospitalization due to a fall and subsequent fractured hip. Prior to her fall she lived at home with her family. Due to the severe decline in her function, she received rehabilitation services for one month prior to the continence program being added to her plan of care. Urinary incontinence had been an issue for years, but got significantly worse over the course of her hospitalization.
Pre-Therapy Status:Urinary Incontinence Frequency: Six episodes per day and three episodes per night.Urinary Sensation: Unable to sense bladder fullness, need to void, or urine loss.Self-Care: Maximal assistance for toileting.
Therapy Information:OmniStim® FX2 Pro Patterned Electrical Neuromuscular Stimulation , OmniCycle® Elite Motorized Therapeutic Exercise SystemFrequency: 5x per week.Protocol Specifics: Continence Improvement program lower extremity triphasic PENSand medium frequency alternating current protocols to improve neuromuscular control forurinary continence. Omnicycle lower extremity neuro mode to increase core and lowerextremity strength.Other Therapy Services Provided: Facilitatory pelvic muscle exercise and functionalmobility exercises.
Read Also: What Causes Urinary Urgency In Females
Relaxation Of Pharyngeal Musculature
Several degenerative neuromuscular diseases result in dysphagic symptoms that require relaxation of pharyngeal musculature. In particular, Parkinsons Disease frequently results in a poorly coordinated, hyper-reactive response of pharyngeal contraction. A patient with this type of diagnosis may demonstrate adequate strength of contraction, but attempts to initiate the swallow results in a characteristic groping behavior. The patient may attempt laryngeal elevation for the swallow numerous times before actual onset and completion of the swallow. Thus, when a swallow is ultimately initiated, the effect is a weakened effort secondary to previously expended energy . The result is an inefficient swallow with an increased risk for post swallow pharyngeal residual and malnutrition secondary to fatigue. In this case the muscles targeted are those responsible for laryngeal elevation . The target behavior is relaxation, rather than contraction, except during the occurrence of the swallow.
The objective of relaxing the pharyngeal musculature before and after the occurrence of a swallow is explained to the patient. After surface electrodes are applied, the patient is instructed to relax the muscles in the neck and throat until the biofeedback line is flat. The patient is then cued to swallow. The target behavior is a flat feedback line with a single peak for the swallow.
REFERENCES
What Does Treatment With Ptns Involve
- Initially 12 treatments are administered at approximately weekly intervals in the consulting rooms.
- Each treatment session lasts about 30 minutes. Treatments do not require any preparation, fasting or restriction in activities such as driving.
- In the seated position a fine needle similar to an acupuncture type needle is inserted into the skin just behind the ankle on the inner aspect of the leg.
- The needle is connected to a device that sends a low-grade electrical signal, which travels up the nerves in the leg to the nerves that control the bladder.
- A tingling sensation may be felt in the ankle, foot or toes during the treatment.
- Further maintenance treatments are required with PTNS
- These usually involve a single treatment that may occur once every few months.
- The ideal long-term treatment frequency is yet to be established and depends on the individuals response to treatment.
You May Like: What Treatment Options Are Available For Urinary Incontinence
How Can Ems Training Help With Incontinence
EMS training of the pelvic floor muscles can relieve or prevent incontinence by strengthening the muscles. If the pelvic floor muscles are too weak due to a lack of exercise, this can lead to a lowering of the internal organs. The bladder and rectum, among others, are affected, which can lead to bladder weakness or incontinence.
Why Does Incontinence Develop

Incontinence can be caused by a number of factors:
- Overweight that presses on the bladder, for example during pregnancy.
- A softening of the connective tissue around the pelvic floor caused by hormonal changes, e.g. during pregnancy or the menopause.
- An overstretching of the pelvic floor during a natural birth .
- Psychosocial burdens e.g. stress.
- Physical stress associated with heavy lifting.
- An enlarged prostate gland or prostate diseases that lead to a narrowing of the urethra.
Don’t Miss: Can Intercourse Cause A Urinary Tract Infection
How Big Is The Device
Medical technology has made significant advances in recent years, and implantable medical devices have gotten smaller. The current device, which is about the size of a thumbnail drive, is smaller than most pacemakers. A new version is available that has a rechargeable battery that lasts about 15 years. These devices also are MRI-safe so you can have scans of your hips, back or legs in the future, if needed.
Electrical Stimulation In Men With Urinary Incontinence After Radical Prostatectomy
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government.Know the risks and potential benefits of clinical studies and talk to your health care provider before participating. Read our disclaimer for details. |
| First Posted : February 11, 2022Last Update Posted : July 12, 2022 |
Aim: In this study, the investigators aimed to assess the efficacy of perineal electrical stimulation on anxiety, depression, quality of life , and clinical parameters associated with incontinence in men with urinary incontinence after radical prostatectomy.
| Not Applicable |
Group 2: No-treatment Subjects in the control group will through baseline assessment and will not receive treatment or instructions to perform pelvic floor exercises at home. After 8 weeks they will submit to the final assessment. After the final evaluation, they will be invited to start treatment in the urogynecological rehabilitation unit.
During the treatment, all men were advised to continue the medical treatment which is not related to incontinence.
Don’t Miss: Tips For Urinary Tract Infection
Modified Valsalva / Effortful Swallows
A common diagnostic finding in the dysphagic population is decreased or weakened contraction of the pharyngeal constrictors responsible for propulsion of the bolus through the pharynx. Weakness of these muscles results in post-swallow pharyngeal residual of the bolus, placing the patient at risk for post swallow aspiration. A modified valsalva swallow, or hard swallow can be used as a compensatory strategy to aid pharyngeal clearing during a meal and also as an indirect exercise for increasing pharyngeal constriction. The superior, middle and inferior constrictors are internal pharyngeal muscles that are not easily accessible by surface electrode. Direct EMG measurement of these muscles is not feasible. Although further investigation is required to specifically document the correlation, clinical practice demonstrates a functional relationship between increased pharyngeal constriction and contraction of the submandibular musculature. Thus, in focusing treatment on increased pharyngeal contraction, the electrodes are placed to target the suprahyoid musculature. This muscle group specifically includes the anterior belly of digastric muscle, the stylohyoid muscle, and the mylohyoid muscle. Collectively, these muscles are responsible primarily for elevation of the larynx and tongue and anterior displacement of the cricoid, hyoid, larynx, trachea and tongue. The stylohyoid adds a component of posterior displacement of the above structures with obliteration of the oropharynx.
Why Do Prostate Treatments Cause Urinary Incontinence
Urine is stored inside the bladder until you have the urge to urinate. The bladder is a hollow, muscular, balloon-shaped organ. Urination happens when:
-
The muscles in the wall of the bladder contract, forcing urine out of the bladder
-
At the same time, muscles that surround the urethra relax and allow the flow of urine
The prostate gland surrounds the urethra. An enlarged prostate gland can obstruct the urethra.
Continence problems may arise as follows:
-
The enlarged prostate can cause urination retention and other problems with urination
-
Removing the prostate through surgery or destroying it through radiation disrupts the way the bladder holds urine and can result in urine leakage
-
Removing or destroying the prostate gland, which is the size of a walnut, initially creates a hole where the gland once was it takes time for this hole to heal over
-
For most men the healing will have closed the hole after approximately 12 months – most men but not every man
-
Radiation can decrease the capacity of the bladder and cause spasms that force urine out
-
Surgery can, at times, damage the muscles and nerves that help control bladder function
Read Also: Doterra Oils For Urinary Tract Infection
What Is Posterior Tibial Nerve Stimulation
Posterior tibial nerve stimulation is a form of neuromodulation i.e. it aims to change the abnormal pattern of stimulation of the nerves that supply the bladder and pelvic floor.
Bladder and pelvic floor muscle function is co-ordinated in the lower part of the spinal cord by the sacral nerves. Electrical stimulation of the posterior tibial nerve sends a message to the sacral nerves that is thought to modify and regulate the nerves that control the bladder.
Functions Of The Male Pelvic Floor
The functions of the pelvic floor are numerous and important. They include:
-
Supporting the organs situated directly above – prostate, bladder, rectum and seminal glands
-
Making an essential contribution to core strength. The pelvic floor is the centre of gravity in your frame – as part of your core muscles it makes a fundamental contribution to movement, back strength and stability
-
Playing an essential role in sexual function – a strong, supple pelvic floor enhances sexual response, improves performance and heightens the sense of pleasure
Also Check: How Are Urinary Tract Infections Caused