B Searching For The Evidence: Literature Search Strategies For Identification Of Relevant Studies To Answer The Key Questions
We will search Ovid Medline, Ovid PsycInfo, Ovid Embase, and the Cochrane Central Register of Controlled Trials to identify randomized controlled trials for primary health outcomes published and indexed in bibliographic databases. We will attempt to assess long-term or rare harms with nonrandomized controlled trials and large controlled observational studies if RCTs are not available. Our search strategy includes relevant medical subject headings and natural language terms for LUTS/BPH . These concepts were combined with filters to select trials. We will supplement the bibliographic database search with forward and backward citation searching of relevant systematic reviews and other key references. We will update searches while the draft report is under public/peer review.
We will search for grey literature in ClinicalTrials.gov and to identify completed and ongoing studies. We will search for conference abstracts from the past three years to identify ongoing studies. Grey literature search results will be used to identify studies, outcomes, and analyses not reported in the published literature. Information from grey literature will also be used to assess publication and reporting bias and inform future research needs. Additional grey literature will be solicited through a notice posted in the Federal Register and Scientific Information Packets and other information solicited through the AHRQ Effective Health Care Web site.
C Data Abstraction And Data Management
Data fields to be extracted will include author, year of publication, sponsorship, setting, subject inclusion and exclusion criteria, intervention and control characteristics, sample size, follow-up duration, participant baseline age, race, and AUA/IPSS scores, and results of primary outcomes and adverse effects. Relevant data will be extracted into web-based extraction forms created in Microsoft Excel. Data will be analyzed in RevMan 5.3 software.19 Data will be extracted to evidence and outcomes tables by one investigator and reviewed and verified for accuracy by a second investigator.
What Are The Most Recent Relevant Guidelines
The most recent evidence-based recommendations in this field are the 2012 Guidelines on the Management of Male LUTS, published by the European Association of Urology . The American Urological Association and the United Kingdoms National Institute for Health and Clinical Excellence published guidelines for BPH and male LUTS, respectively, in 2010., Finally, the recommendations of the International Scientific Committee on the Evaluation and Treatment of Lower Urinary Tract Symptoms in Older Men were published in 2009.
Recommended Reading: Can Clarithromycin Be Used To Treat A Urinary Tract Infection
The International Prostate Symptom Score
All men with lower urinary tract symptoms should complete the International Prostate Symptom Score survey, consisting of seven questions about urinary symptoms plus one about quality of life. Specifically, it asks the patient, âOver the past month, how often have youâ¦â
-
Had a sensation of not emptying your bladder completely after you finish urinating?
-
Had to urinate again less than 2 hours after you finished urinating?
-
Found you stopped and started again several times when you urinated?
-
Found it difficult to postpone urination?
-
Had a weak urinary stream?
-
Had to push or strain to begin urination?
Each question above is scored as 0 , 1 , 2 , 3 , 4 .
-
Over the past month, how many times did you most typically get up to urinate from the time you went to bed until the time you got up in the morning?
This question is scored from 0 to 5 .
-
If you were to spend the rest of your life with your urinary condition the way it is now, how would you feel about that?
This question is scored as 0 , 1 , 2 , 3 , 4 , 5 , or 6 .
A total score of 1 to 7 is categorized as mild, 8 to 19 moderate, and 20 to 35 severe.
The questionnaire can also be used to evaluate for disease progression and response to treatment over time. A change of 3 points is clinically significant, as patients are unable to discern a difference below this threshold.
Personal And Family Medical History
Taking a personal and family medical history is one of the first things a health care provider may do to help diagnose benign prostatic hyperplasia. A health care provider may ask a man
- what symptoms are present
- when the symptoms began and how often they occur
- whether he has a history of recurrent UTIs
- what medications he takes, both prescription and over the counter
- how much liquid he typically drinks each day
- whether he consumes caffeine and alcohol
- about his general medical history, including any significant illnesses or surgeries
Don’t Miss: Where To Buy Azo Urinary Pain Relief
Important Points In Treatment
Much of the âtreatmentâ for benign prostatic hypertrophy is watchful waiting. Not every man with prostatic hypertrophy requires medical or surgical treatment.
One treatment for benign prostatic hypertrophy is surgery. Usually, this is done through the urethra, the opening in the penis, and it does not leave an external scar. Your physician can review with you the benefits and risks of this form of therapy.
Alternatively, there are two medical therapies that can benefit some patients. One drug, finasteride , acts by decreasing the level of a male hormone in the prostate gland. This slows the growth of the prostate gland, and, in many cases, the gland shrinks. Symptoms improve if the gland shrinks adequately. Not all patients note an improvement in symptoms. Improvement may take 6 months or more. This drug has few side effects. A few patients experience decreased sex drive.
Terazosin , and other drugs of this sort, is of use in some men with benign prostatic hypertrophy. This drug is used for the treatment of high blood pressure. It relaxes the muscles in the blood vessels, allowing the blood pressure to fall. It can also relax the muscles where the bladder empties, reducing the obstruction caused by the enlargement of the prostate gland. It is more rapidly effective than finasteride. This medication does have side effects, particularly faintness on standing.
Although both finasteride and terazosin are effective, they are suitable for use in some patients only.
Other Invasive Surgical Procedures
Transurethral Incision of the Prostate
In TUIP, the surgeon makes only one or two incisions in the prostate, causing the bladder neck and the prostate to spring open and reduce pressure on the urethra. TUIP is generally reserved for men with minimally enlarged prostates who have obstruction of the neck of the bladder.
TUIP is less invasive than TURP, has a lower rate of the same complications , and usually does not require a hospital stay. More studies are still needed, however, to determine whether they are comparative in long-term effectiveness.
Simple Prostatectomy
In simple prostatectomy, the enlarged prostate is removed through an open incision in the abdomen using standard surgical techniques. This is major surgery and requires a hospital stay of several days. Simple prostatectomy is used only for severe cases of BPH, when the prostate is severely enlarged, the bladder is damaged, there are many stones or one large stone in the bladder, or other serious problems exist. Some people need a second operation because of scarring. Side effects of simple prostatectomy can include erectile dysfunction and urinary incontinence. This surgery can be performed through an incision in the lower abdomen or keyhole incisions for robot-assisted laparoscopy.
Also Check: What Foods Cause Urinary Tract Infections
Sidebar 1 Bph Case Report
Chief Complaint: LF is a 64-year-old white male presenting with fatigue and sleep pattern changes that have lasted over the past several years. He believes his poor sleep habits are due to frequent nighttime urination, occurring three to four times per night. He denies drinking any fluids in the evening. LF also complains of difficulty starting a stream, especially in public restrooms, and notes that this stream has become weaker over time. He also feels that it takes him longer to completely empty his bladder. He admits to âgoing a little in his shortsâ after urinating and confirmed postvoid dribbling. He experiences some mild urgency but denies dysuria. He also confirms knowledge of all of the bathroom locations in his office building.
Past Medical History: LF denies blood in his urine, a past history of STDs, or other UTIs. He reluctantly reports difficulty keeping firm erections during sexual intercourse compared to when he was younger. However, he maintains that this issue is not one of his major concerns.
Family History: Negative family history of prostate cancer
Social History: Nonsmoker, no illicit drugs, mild alcohol consumption
Physical Examination: Male pattern baldness
Vital Signs: WNL
⢠Niacin 1,000 mg 1 daily
⢠Cinnamon tablet 1 daily
Two Mechanisms: Static Dynamic
BPH is a histologic diagnosis of proliferation of smooth muscle, epithelium, and stromal cells within the transition zone of the prostate, which surrounds the proximal urethra.
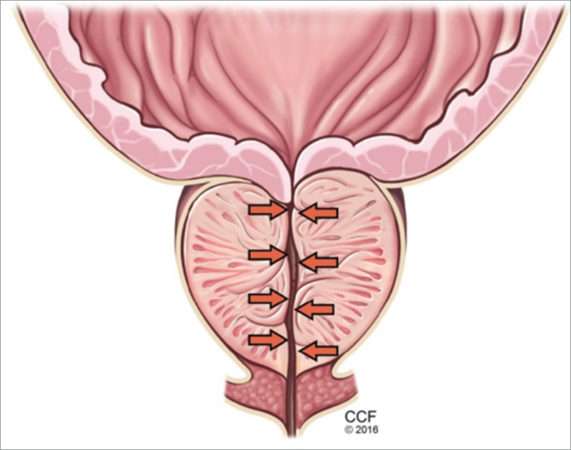
Symptoms arise through two mechanisms: static, in which the hyperplastic prostatic tissue compresses the urethra and dynamic, with increased adrenergic nervous system and prostatic smooth muscle tone . Both mechanisms increase resistance to urinary flow at the level of the bladder outlet.
The static component of benign prostatic hyperplasia and lower urinary tract symptoms, with hyperplasia leading to urethral compression.
The dynamic component of benign prostatic hyperplasia. The bladder outlet and prostate are richly supplied with alpha-1 receptors , which increase smooth muscle tone, promoting obstruction to the flow of urine. Alpha-1 adrenergic blockers counteract this effect.
As an adaptive change to overcome outlet resistance and maintain urinary flow, the detrusor muscles undergo hypertrophy. However, over time the bladder may develop diminished compliance and increased detrusor activity, causing symptoms such as urinary frequency and urgency. Chronic bladder outlet obstruction can lead to bladder decompensation and detrusor underactivity, manifesting as incomplete emptying, urinary hesitancy, intermittency , a weakened urinary stream, and urinary retention.
Don’t Miss: Why Do I Get Urinary Tract Infections Often
Guidelines For The Treatment Of Benign Prostatic Hyperplasia
Yunuo Wu, PharmDCreighton University School of Pharmacy and Health Professions
Michael H. Davidian, MD, MSAssociate Professor of MedicineCreighton University School of Medicine
Edward M. DeSimone II, RPh, PhD, FAPhAProfessor of Pharmacy SciencesCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016 41:36-40.
ABSTRACT:Benign prostatic hyperplasia is a common disorder in men with an incidence that increases with age. BPH often requires therapy when patients begin to experience lower urinary tract symptoms that affect quality of life. Current management strategies involve lifestyle modifications, pharmacotherapy, phytotherapy, and surgical interventions as indicated. Pharmacists are in the unique position of being accessible sources of healthcare information for the BPH patient population. Understanding the symptoms of this disorder and therapy options will be beneficial for pharmacists who have increased chances to answer BPH-related questions from their patients.
Most Men Eventually Develop Bph
Autopsy studies have shown that BPH increases in prevalence with age beginning around age 30 and reaching a peak prevalence of 88% in men in their 80s. This trend parallels those of the incidence and severity of lower urinary tract symptoms.
In the year 2000 alone, BPH was responsible for 4.5 million physician visits at an estimated direct cost of $1.1 billion, not including the cost of pharmacotherapy.
Read Also: How Can A Woman Get A Urinary Tract Infection
Bph Tends To Progress
Understanding the natural history of BPH is imperative to appropriately counsel patients on management options, which include watchful waiting, behavioral modification, pharmacologic therapy, and surgery.
In a randomized trial, men with moderately symptomatic BPH underwent either surgery or, in the control group, watchful waiting. At 5 years, the failure rate was 21% with watchful waiting vs 10% with surgery . In the watchful-waiting group, 36% of the men crossed over to surgery. Men with more bothersome symptoms at enrollment were at higher risk of progressing to surgery.
In a longitudinal study of men with BPH and mild symptoms , the risk of progression to moderate or severe symptoms was 31% at 4 years.
The Olmsted County Study of Urinary Symptoms and Health Status Among Men found that the peak urinary flow rate decreased by a mean of 2.1% per year, declining faster in older men who had a lower peak flow at baseline. In this cohort, the IPSS increased by a mean of 0.18 points per year, with a greater increase in older men.
Though men managed with watchful waiting are at no higher risk of death or renal failure than men managed surgically, population-based studies have demonstrated an overall risk of acute urinary retention of 6.8/1,000 person-years with watchful waiting. Older men with a larger prostate, higher symptom score, and lower peak urinary flow rate are at higher risk of acute urinary retention and progression to needing BPH treatment.,
What Is Benign Prostatic Hyperplasia
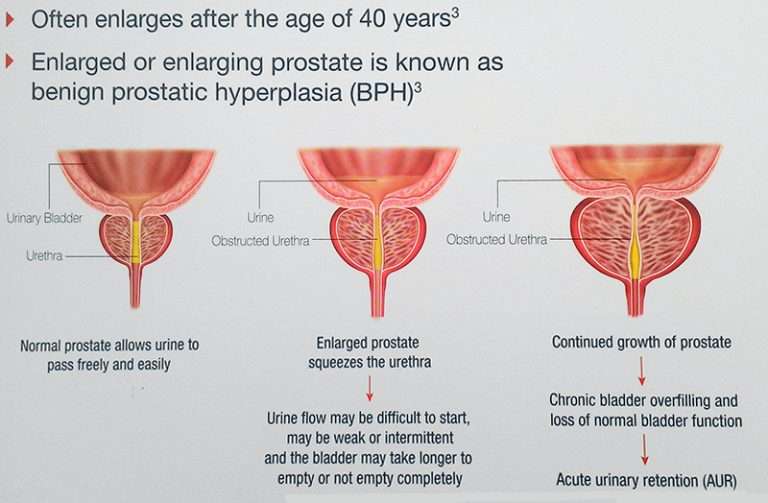
Benign prostatic hyperplasiaalso called BPHis a condition in men in which the prostate gland is enlarged and not cancerous. Benign prostatic hyperplasia is also called benign prostatic hypertrophy or benign prostatic obstruction.
The prostate goes through two main growth periods as a man ages. The first occurs early in puberty, when the prostate doubles in size. The second phase of growth begins around age 25 and continues during most of a mans life. Benign prostatic hyperplasia often occurs with the second growth phase.
As the prostate enlarges, the gland presses against and pinches the urethra. The bladder wall becomes thicker. Eventually, the bladder may weaken and lose the ability to empty completely, leaving some urine in the bladder. The narrowing of the urethra and urinary retentionthe inability to empty the bladder completelycause many of the problems associated with benign prostatic hyperplasia.
Read Also: Upper Urinary Tract Infection Symptoms
What Is The Prostate
The prostate is a walnut-shaped gland that is part of the male reproductive system. The main function of the prostate is to make a fluid that goes into semen. Prostate fluid is essential for a mans fertility. The gland surrounds the urethra at the neck of the bladder. The bladder neck is the area where the urethra joins the bladder. The bladder and urethra are parts of the lower urinary tract. The prostate has two or more lobes, or sections, enclosed by an outer layer of tissue, and it is in front of the rectum, just below the bladder. The urethra is the tube that carries urine from the bladder to the outside of the body. In men, the urethra also carries semen out through the penis.
Other Less Invasive Procedures
These minimally invasive procedures carry fewer risks for incontinence or problems with sexual function than invasive procedures, but it is unclear how effective they are in the long term.
Transurethral Microwave Thermotherapy
Transurethral microwave thermotherapy delivers heat using microwave pulses to destroy prostate tissue. A microwave antenna is inserted through the urethra with ultrasound used to position it accurately. The antenna is enclosed in a cooling tube to protect the lining of the urethra. Computer-generated microwaves pulse through the antenna to heat and destroy prostate tissue. When the temperature becomes too high, the computer shuts down the heat and resumes treatment when a safe level has been reached. The procedure takes 30 minutes to 2 hours, and the patient can go home immediately afterward.
Transurethral Needle Ablation
Transurethral needle ablation is a relatively simple and safe procedure, using needles to deliver high-frequency radio waves to heat and destroy prostate tissue.
Transurethral Electrovaporization
Transurethral electrovaporization uses high voltage electrical current delivered through a resectoscope to combine vaporization of prostate tissue and coagulation that seals the blood and lymph vessels around the area. Deprived of blood, the excess tissue dies and is sloughed off over time.
Water Vapor Thermal Therapy
Read Also: I Think I Have A Urinary Tract Infection
Pelvic Floor Muscle Training
Pelvic floor muscle exercises, also called Kegel exercises, may help men prevent urine leakage, particularly after surgical procedures. These exercises strengthen the pelvic floor muscles that both support the bladder and close the sphincter.
Performing the Exercises
Since the pelvic floor muscles are internal and sometimes hard to isolate, doctors often recommend practicing while urinating:
- Contract the muscle until the flow of urine is slowed or stopped. Attempt to hold each contraction for 20 seconds.
- Release the contraction.
- In general, people should perform 5 to 15 contractions, 3 to 5 times daily.
- Once you are comfortable with pelvic floor exercises, it is best NOT to practice while urinating.
Transurethral Resection Of The Prostate
Transurethral resection of the prostate involves surgical removal of the inner portion of the prostate, where BPH develops. It is the most common surgical procedure for BPH, although the number of procedures has dropped significantly over the past decades because of the increased use of effective medications and the increasing use of alternate procedures.
Procedure
The surgeon inserts a thin fiber-optic tube called a resectoscope into the urethra. No incision or stitches are needed. The resectoscope is a type of endoscope. It has a telescope lens to help the surgeon see the prostate gland. The surgeon uses a wire cutting loop inserted into the resectoscope to cut away excess prostatic tissue using a monopolar electrocautery, and fluid irrigation solutions are used to flush away the excised matter. TURP can be done as an outpatient procedure but may require a 1 to 2 day hospital stay. A newer version called bipolar TURP uses a bipolar electrocautery instead which allows the use of saline as the irrigation solution.
A Foley catheter generally remains in place for 1 to 3 days after surgery to allow urination. This device is a tube inserted through the opening of the penis to drain the urine into a bag. The catheter can cause temporary bladder spasms that can be painful. The catheter may be removed while the person is in the hospital or after they are sent home.
Recuperation
Complications
Immediate short-term complications after surgery may include:
Don’t Miss: Urinary Incontinence After Prostate Surgery
A Criteria For Inclusion/exclusion Of Studies In The Review
Studies will be included in the review based on the PICOTS framework outlined above and the study-specific inclusion criteria described in Table 3.
|
|
| Publication type | |
|---|---|
| Language of Publication | English |