Future Perspectives And Conclusions
Prostate cancer is one of the most problematic and frequently encountered malignancies in male patients. It often occurs when men are still in the active period of their lives. Consequently, there is a high demand for minimally invasive therapeutic approaches, susceptible of preserving urinary continence and sexual function. Unfortunately, stress urinary incontinence is a common adverse event in men with localized or locally advanced prostate cancer undergoing radical prostatectomy, but also secondary to radiotherapy and to cryosurgery .
Despite rehabilitative procedures such as pelvic floor muscle training, biofeedback, electrical stimulation, lifestyle changes, or a combination of these strategies, no fully efficient treatment alternative has yet been established for this pathology . On the other hand, it should be acknowledged that nursing care, including the understanding of the patient’s needs, education, and psychosocial support remain essential features while aiming to improve the quality of life of prostate cancer patients.
The Truth About Incontinence After Prostate Cancer
The realities of a prostate cancer diagnosis extend well beyond the need for treatment decisions. Rumors abound regarding the risk of damage to urinary control and sexual potency functions that are core to a mans well-being and sense of worth. But the prospect of living with incontinence after prostate cancer surgery does not have to be the ominous cloud men fear. The decisions a man makes about treating prostate cancer, the preparations for that treatment and the follow-up care received each have a great impact on a mans urinary health.
For most men, robotic prostatectomy surgery is the best form of prostate cancer treatment. Complete removal of the prostate and surrounding cancer offers men the strongest chance of cure and survival. But as with many cancers, treatment can bring the bad with the good. Some degree of urinary incontinence after prostate surgery, though often short-term, is a reality of recovery.
Exercise Your Pelvic Floor Muscles
Learning how to control the pelvic floor muscles can speed up the recovery process and reduce leakage. If you don’t strengthen these muscles, the leakage may persist.
Please note: Performing pelvic floor muscle exercises before and after prostate surgery is vital to your recovery. Resume pelvic floor exercises once the catheter has been removed to avoid bladder irritation and discomfort. It is recommended that you seek help from a mens, womens and pelvic health physiotherapist, Nurse Continence Specialist, or urology nurse to learn the correct technique.
More information about the pelvic floor muscles can be found on our pelvic floor and male pelvic floor pages. You can also learn more about pelvic floor friendly exercises at pelvicfloorfirst.org.au.
Also Check: Amoxicillin For Urinary Tract Infection
How Much Urinary Incontinence Will You Experience After Prostate Surgery
The type of urinary incontinence most often experienced by prostate cancer survivors is called stress incontinence. As a result of disruption or damage during surgery, the sphincter muscles that control the release of urine may be weakened. The level of incontinence varies some men may have slight leaking or dripping, while others may experience complete bladder emptying. This unwanted release of urine can happen at any time. Strenuous activities and sports are a culprit, or a simple laugh, cough, sneeze or change of position may trigger it. Biologically, this type of incontinence is actually very similar to what some women experience post-childbirth. For men who choose radiation therapy, a different type of incontinence called urge incontinence may be experienced. Urge incontinence is characterized by frequent urination and the urge to go immediately, resulting in not being able to get to the restroom fast enough.
Continence After Prostate Cancer Surgery How Long Does It Last
A prostatectomy is a procedure that can affect a man both physically and emotionally. Undergoing such a surgery may come with various reasons for anxiety and fear. Incontinence may be one of them.
The prostate is an important gland in the body that regulates many physical functions, including the urinary and sexual functions. Once removed through radical prostatectomy, negative side-effects may result. The most common reasons for concern are:
- Urinary incontinence
- Sexual dysfunction
You May Like: Hills Urinary Care C D Multicare
Evaluation Of Incontinence After Prostate Treatment
Guideline Statement 9
Clinicians should evaluate patients with incontinence after prostate treatment with history, physical exam, and appropriate diagnostic modalities to categorize type and severity of incontinence and degree of bother.
Discussion
There is no formal evidence regarding the effects of history and physical exam on outcomes of IPT treatments however, there is universal agreement that taking a history and performing a physical examination should be the first step in the assessment of anyone with urinary incontinence.73 There is strong evidence that a history of pelvic RT74,75 is associated with the severity of incontinence, especially stress incontinence,76,77 after prostate surgery.
The Panel believes that before treating IPT, it is critical to categorize the type of incontinence and the severity and degree of bother of incontinence. The status of prostate cancer also should be known, particularly for men who are candidates for salvage RT, which may impact efficacy of continence treatment.
History is the first step in determining the type of incontinence, which is important because treatments for SUI and urgency incontinence are very different. In cases of mixed incontinence, it can be important to determine which component is more prevalent and bothersome, though many investigators feel that treatment outcomes for urgency incontinence may be difficult to determine in the face of significant sphincteric insufficiency.
Guideline Statement 10
Discussion
What Treatments Are Available To Me If My Incontinence Doesnt Go Away After A Year
While kegels and behavioral therapy work well for most men with mild to moderate leaking, they may not be completely effective for some. Luckily, there are still some options for treating bladder leakage after prostate surgery.
Another surgery is sometimes needed when bladder leaks persist for more than a year after surgery. This may consist of having a urethral sling procedure, or an artificial urinary sphincter.
With a urethral sling procedure, a synthetic mesh tape is implanted to support the urethra. Up to an 80% improvement has been seen with this procedure and some men stop leaking completely.
An artificial urinary sphincter is used in patients who have more severe urinary incontinence that is not improving, or for those patients who may have had a lot of damage to the sphincter muscle after prostate surgery. An artificial urinary sphincter is a mechanical ring that helps close the exit from the bladder.
As will all surgeries, these come with pros and cons and potential complications. Be sure to discuss these options with your doctor.
You May Like: Drugs To Control Urinary Incontinence
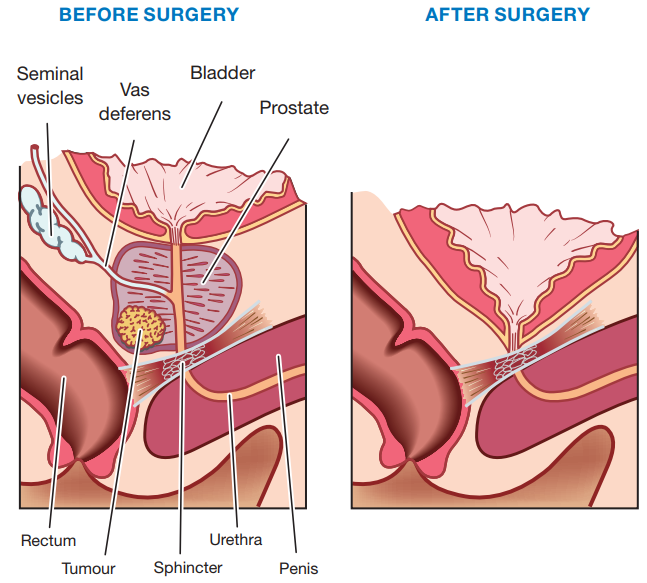
Why Do Prostate Cancer Treatments Cause Urinary Incontinence
It helps to know a bit about how the bladder holds urine. When urine is emptied into the bladder from the kidneys, it is stored inside the bladder until you have the urge to urinate. The bladder is a hollow, muscular, balloon-shaped organ. Urine flows out of the bladder, and leaves the body through a tube called the urethra. Urination happens when the muscles in the wall of the bladder contract, forcing urine out of the bladder. At the same time, muscles that surround the urethra relax and allow the flow of urine. The prostate gland surrounds the urethra. Because an enlarged prostate gland can obstruct the urethra, it can cause urination retention or other problems with urination.
Removing the prostate through surgery or destroying it through radiation can disrupt the way the bladder holds urine and can result in urine leakage. Radiation can decrease the capacity of the bladder and cause spasms that force urine out. Surgery can, at times, damage the nerves that help control bladder function.
Risk Of Bias Assessment
The Newcastle Ottawa scale, which evaluates cohort selection, comparability and outcomes assessment, was used for non-randomized controlled trials . The Cochrane risk of bias tool which evaluates random sequence generation, allocation concealment, blinding, and attrition was used for evaluation of RCTs.
Read Also: Severe Urinary Tract Infection Symptoms In Elderly
Treating Urinary Incontinence After Prostate Surgery
Up to 10 percent of men will experience some degree of urinary incontinence after prostate cancer surgery, says Benjamin McCormick, a University of Utah Health surgeon specializing in reconstructive urology. It occurs because part of the continence mechanism may have to be removed to treat the prostate cancer. McCormick says it can leave the patient with something called stress incontinence.
Under the umbrella of incontinence, there are three main types, says McCormick.
- Stress incontinence, which is urine leakage associated with activity
- Overflow incontinence, where the bladder is full but theres no sensation, so it spills over
- Urge incontinence, also known as an overactive bladder
Statistics On Incontinence After Surgery
A large number of men experience incontinence after a total prostatectomy, at least temporarily. For some lucky few, the incontinence will end in a short time, others will suffer for a few months, and some may live with it permanently.
Many doctors tend to maximize the small number of patients that have few problems and ignore the larger numbers that have permanent dysfunction.
Generally, a Foley catheter is inserted during or just before the surgery to take care of temporary incontinence caused by the surgery. This device will be left in the patient for about a week after surgery.
A Foley catheter is a flexible tube that is passed through the penis and into the bladder to drain urine. It is held in place in the bladder by a small balloon inflated at insertion time. Its other end connects to a collection bag. It is an indwelling urinary catheter designed for short-term use.
On a follow-up visit after surgery, the surgeon will remove the Foley catheter, and the man can attempt natural voiding. In many cases, natural voiding is unsuccessful, and the catheter is left in for another cycle. Usually, the patient is introduced to absorbent pads as a temporary measure until natural voiding is successful.
Recommended Reading: Sacral Nerve Stimulation For Urinary Incontinence
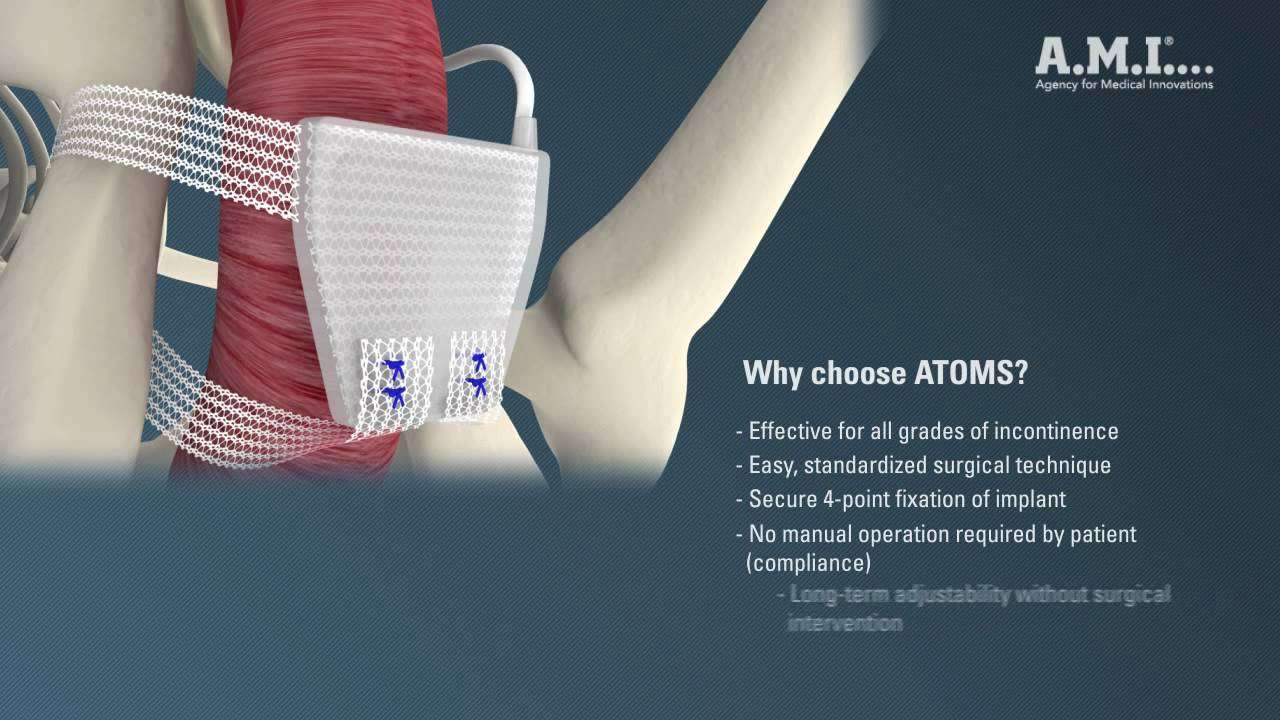
Surgical Approaches: Artificial Urinary Sphincter
Surgical intervention for incontinence is typically deferred for at least one year following prostatectomy. Traditionally, the AUS has been the gold standard surgical treatment for SUI after prostatectomy since its introduction several decades ago, offering the advantage of both durability and effectiveness for even severe degrees of incontinence. Initially conceptualized by Foley in 1947, the modern AUS design has evolved over several iterations, with closer resemblance to designs introduced in the 1970s by Scott and Rosen. The present models are fashioned on the concept of using an inflatable fluid-filled cuff surrounding the urethra to control continence in addition to a hydraulic pressure-regulating balloon reservoir and control pump. In the resting activated state, the cuff is inflated, thereby occluding the urethra. When the control pump, implanted in the scrotum, is squeezed manually, the cuff is deactivated. This pumps fluid out of the cuff into the reservoir, thereby depressurizing the cuff and enabling the patient to void. Unless locked in the deactivated state, the cuff automatically reactivates over the subsequent 45 to 90 seconds following deactivation to prevent further flow of urine through the urethra.
What Kinds Of Surgeries Treat Urinary Incontinence After Your Prostate Is Removed
There are two types of surgery for urinary incontinence: the urethral sling and the artificial urinary sphincter. Usually, the incontinence needs to last for about one year after the prostatectomy to be sure there is not going to be further improvement before your healthcare provider suggests this type of therapy.
Also Check: Physical Therapy For Urinary Incontinence
What Is An Artificial Urinary Sphincter And How Does It Help With Urinary Incontinence
An artificial urinary sphincter can help men who have moderate to severe urinary incontinence due to poorly functioning muscle or sphincter valve after prostate cancer surgery.
The AUS has three parts:
- An inflatable cuff that is placed around the upper urethra. The cuff closes off the urethra to prevent leakage of urine.
- A pump that is inserted into the scrotum. It’s completely on the inside and not visible, and the pump controls the opening and closing of the cuff.
- A small pressure-regulating balloon that is placed in the abdomen, under the muscles. The balloon maintains fluid under pressure within the urethral cuff to pressurize the system and hold urine back.
If you have this surgery, youll press on the pump when you feel the need to pee. This opens the cuff to allow urine to pass. When youre done peeing, the cuff automatically closes again on its own.
The AUS procedure provides a very good and satisfactory result in 90% of cases. Risks are uncommon and include:
- Failure of the device .
- Erosion of the cuff into the urethra.
- Infection.
All of these would require additional surgery.
What Is Urinary Incontinence And How Is It Related To Prostate Cancer Surgery
Urinary incontinence is the loss of the ability to control urination . Urinary incontinence sometimes occurs in men who’ve had surgery for prostate cancer.
If youve had prostate cancer surgery, you might experience stress incontinence, which means you might leak urine when you cough, sneeze or lift something that is heavy. This happens because of stress or pressure on the bladder. There is also a type of incontinence that is called urge incontinence. When this happens, you are hit with a sudden need to urinate right away and have leakage before you can make it to the bathroom.
Recommended Reading: What Can You Do For Urinary Incontinence
The Results Were Impressive
A whopping 87 percent found that their incontinence improved with this targeted approach. And, 58 percent achieved what is considered the optimal level of improvement needing two or fewer protective pads per day.
The benefits didnt stop their either
The men receiving individualized therapy based on their muscle issues also reported a decrease in pain. In fact, while 27 percent were suffering at the beginning of the study, that number dropped to just 14 percent after only four sessions.
While this may not seem like a huge decrease, according to the researchers, it was actually quite impressive.
This is the first study to show a decrease in post-prostatectomy pain after therapy, said Kelly M. Scott, M.D., an associate professor in the Department of Physical Medicine and Rehabilitation at UT Southwestern and first author of the study.
Aua Nomenclature: Linking Statement Type To Evidence Strength
Where gaps in the evidence existed, the Panel provides guidance in the form of Clinical Principles or Expert Opinions with consensus achieved using a modified Delphi technique if differences of opinion emerged.2 A Clinical Principle is a statement about a component of clinical care that is widely agreed upon by urologists or other clinicians for which there may or may not be evidence in the medical literature. Expert Opinion refers to a statement, achieved by consensus of the Panel, that is based on members’ clinical training, experience, knowledge, and judgment for which there is no evidence.
Don’t Miss: Can Cranberry Juice Cure A Urinary Tract Infection
‘just Cant Wait’ Card
You can get a card to show to staff in shops or pubs etc. It allows you to use their toilets, without them asking awkward questions. You can get the cards from Disability Rights UK or the Bladder and Bowel Community. They also have a map of all the public toilets in the UK.
You could get a key to disabled toilets if you need to access them quickly. You buy the RADAR key from Disability Rights UK. But this should only be used by people who need quick access to a disabled toilet due to a disability or medical condition.
Is It Normal To Have Urinary Frequency After A Turp
Urinary frequency after TURP is a common occurrence. Yes in many cases it will settle down, but in others it may not. That is why some men have serious long-term side effects.
TURP Surgery What is a TURP ? Transurethral Resection of the Prostate , is a surgical procedure used to treat urinary symptoms due to BPH .
Read Also: Ways To Get Rid Of Urinary Tract Infection
Are There New Techniques That Reduce The Chance Of Becoming Incontinent
When removingthe prostate, surgeons try to save as much of the area around the bladder and the sphincter muscles around the urethra as possible, thus limiting damage to the sphincter. Doctors have also fine-tuned the process of placing radioactive seed implants, using sophisticated computer projections that allow the seeds to destroy the prostate while limiting damage to the bladder.
Still, at this point, any man who is undergoing radiation or surgery to treat prostate cancer should expect to develop some problems with urinary control. With newer techniques, some men will have only temporary problems controlling their urine, and many will regain full control of their bladder in time.
Continued
Over The Counter For Bladder Control
So, whats available to men OTC for bladder control?
For incontinence care at home, there’s a device called a Cunningham Clamp that can be used very temporarily, says McCormick. It’s just a soft clip that stays on the penis and can help hold back urine. The user decides when to remove it, to relieve themselves.
The bladder is supported by pelvic floor muscles, so in some patients stress incontinence can be improved by simple light pelvic exercises to restore flexibility and muscle strength. McCormick says Its also helpful to drink enough water and avoid caffeine and alcohol.
You May Like: What Do You Do For A Urinary Tract Infection
Conservative And Pharmacologic Therapy
Although there is conflicting evidence regarding the importance of conservative treatment after post-prostatectomy urinary incontinence , pelvic floor muscle training is still considered as the first treatment choice . Duloxetin, a serotonin/norepinephrine reuptake inhibitor, either alone or in combination with PFMT, may hasten recovery of urinary incontinence but is often associated with severe gastrointestinal and central nervous side effects . However, neither PFMT nor duloxetine may cure male stress urinary incontinence.
How Long Does It Take For Turps To Come Out
TURP recovery is usually complete after two months. Men who still have trouble voiding urine may need to stay on medications or undergo additional surgeries. Occasional checkups with a doctor are important to keep a close eye on changes in prostate health.
If you have no control post op it could be one of four things going on: You could be in retention causing urinary frequency, urgency and incontinence.
Don’t Miss: Urinary Tract Infection Immediate Relief