What Will Happen During The Second Stage Of Sns
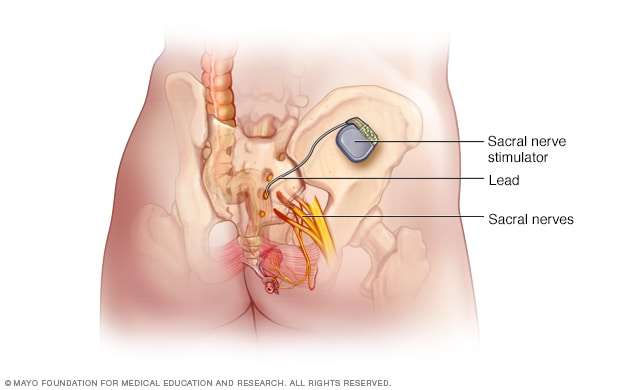
You may be given general anesthesia to keep you asleep and free from pain during the procedure. You may instead be given local anesthesia to numb the procedure area. With local anesthesia, you may still feel pressure or pushing during the procedure, but you should not feel any pain. You will be placed on your stomach. Your healthcare provider will reopen the incision that was made during the first stage. A space is made just under your skin. The stimulator is connected to a permanent lead. Then, the stimulator is placed into the space and the space is closed with stitches. You will be given a programming device to adjust and turn the stimulator off and on as needed.
How Do I Prepare For Sacral Nerve Stimulation
Your healthcare provider will talk to you about how to prepare for each stage of this procedure. He or she may tell you not to eat or drink anything after midnight on the day of your procedure. He or she will tell you what medicines to take or not take on the day of your surgery. You may be given an antibiotic through your IV to help prevent a bacterial infection.
Literature Review: Objectives And Methods
The Medical Advisory Secretariat did a cost analysis of SNS for the management of urinary urge incontinence, urgency-frequency, urinary retention, and fecal incontinence. Previous health technology assessments and the peer-reviewed literature from 2000 to January 2005 were searched using the keywords listed in the methods for the literature review.
Don’t Miss: Urinary Tract Infection Foods To Avoid
How Well It Works
Vaginal or anal electrical stimulation has been tried mostly in women who have urge, stress, and mixed incontinence. There is some research that it can help reduce how often women have incontinence.footnote 1
In men who had been incontinent for a year after prostatectomy, pelvic floor exercises and anal electrical stimulation did not improve incontinence any more than pelvic floor exercises alone after 8 weeks.footnote 2
Posterior tibial nerve stimulation may help about half of the people who get it. In one study, about 5 out of 10 people who had the treatment were better after 12 weeks.footnote 3
Sacral nerve stimulation has been studied for urge urinary incontinence that hasn’t gotten better with other treatments. Most of the studies have only included a small number of women. In those studies, about half of women had some improvement in urinary incontinence after treatment.footnote 4
Interstim Continence Control Therapy / Sacral Nerve Stimulation

Don’t Miss: Can Probiotics Help With Urinary Tract Infection
Evolution Of The Procedure
Direct neural stimulation to produce a clinical effect was first hypothesized as long ago as 1906 . Experimental work using SNS for functional disturbances of micturition began in the 1950s, with stimulation of the spinal cord, the detrusor muscle and the striated sphincter used to try and provoke controlled micturition . The first clinical application of these principles was an SNS implant performed in 1981 by Tanagho and Schmidt . In 1990, Brindley reported his technique for anterior sacral nerve root stimulation in patients with urinary dysfunction secondary to chronic spinal injury. With these insensate patients, short-lived high-voltage stimulation could be employed to produce tetanic contraction of bladder and sphincter. Once the stimulus was removed, the fast twitch sphincter muscle relaxed quickly and the slow twitch detrusor relaxed slowly, thereby creating a pressure differential to facilitate micturition. Bowel function was also affected in these patients, with the induction of peristaltic, frequency-dependant, high-pressure colorectal contractions.
The Brindley technique causes pain in patients with an intact spinal cord. Therefore, chronic stimulation at low amplitude, or neuromodulation, was employed for urological dysfunction in these patients. This evolved to the current indication: SNS to control voiding difficulties and urinary incontinence when the urinary tract seems to be structurally intact, but functionally deficient .
The Science Behind Sacral Neuromodulation
One way the brain controls our bodys muscles and movements is through electrical messages, which are carried by nerves. These nerves have major routes with smaller pathways running off them.
One major route runs from the brain, along the spinal cord and through the lower back called the sacral area. Here, nerve paths split off and go in different directions, some to the pelvic area. The muscles in the pelvic area, such as the pelvic floor, urethral sphincters, bladder and anal sphincter muscles are controlled by the brain through nerves that run from the sacral area. Our sensations, such as fullness in the bladder or rectum, are also relayed to the brain via these nerve routes.
Sacral Neuromodulation helps to correct inappropriate, unwanted or even erroneous messages sent along these nerve pathways.
Recommended Reading: Can Baking Soda Cure Urinary Tract Infection
Staged Implant Retrospective Study
This was a retrospective study conducted in patients who had inconclusive test stimulation results with the Medtronic model 3057 test stimulation lead. In this study, the test stimulation typically lasted for 3-5 days, but no more than 7 days. Participating physicians reported that 76 of the 80 patients had a successful screening period with the staged implant. Of the 80 patients screened, 73 went on to undergo Interstim implantation, 60 of whom were noted to have a successful outcome during an average follow-up of 1.6 years . Of the 80 patients who were screened with a long-term lead for a staged implant, 47 had also been screened with a temporary model 3057 test stimulation lead.
Test stimulation was unsuccessful with the model 2057 lead in 24 of the 47 patients prior to receiving the staged implant. Screening with the long-term lead was successful in 21 of these 24 patients. Thus, it appears that use of the long-term lead for screening as part of a staged implant may be helpful in patients with inconclusive results from screening with the model 3057 lead, to determine if they will benefit from Interstim implantation.
What Is Sacral Nerve Stimulation
Nerve stimulation is a reversible treatment for patients with bladder control problems in whom conservative treatments have not worked or have not been tolerated. Conservative treatments include behavioral therapies and medications.
- Urinary Urgency failure to be able to postpone the need to urinate
- Frequency of Urination the need to urinate at least eight times per day
- Urge Incontinence leakage of urine when one gets the urge to urinate
Sacral nerve stimulation also addresses the problem of nonobstructive urinary retention, a urinary condition defined by such markers as the need for a catheter to pass urine spending considerable time in the bathroom, yet only able to produce a weak, dribbling stream of urine urinary leakage and not having a sensation that your bladder is full.
Additionally, sacral nerve stimulation is now FDA-approved for men and women with accidental bowel leakage, or fecal incontinence.
Sacral nerve stimulation will not alway cure these bladder and bowel control problems but it can reduce the number of voidsand/or the number of wetting or incontinent episodes.
You May Like: Tea For Urinary Tract Health
License For Use Of Current Dental Terminology
End User License Agreement:These materials contain Current Dental Terminology , copyright © 2020 American Dental Association . All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled I accept, you hereby acknowledge that you have read, understood and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled I do not accept and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, you and your refer to you and any organization on behalf of which you are acting.
What Will Happen During The First Stage Of Sns
You may be given general anesthesia to keep you asleep and free from pain during the procedure. You may instead be given local anesthesia to numb the procedure area. With local anesthesia, you may still feel pressure or pushing during the procedure, but you should not feel any pain. You will be placed on your stomach. A small incision will be made in your upper buttock. A temporary or permanent lead is placed into your lower back, through to your sacral nerves. Your incision will be closed with surgical glue or tape. The lead is connected to an external stimulator. Electrical impulses will be sent to the lead to stimulate your sacral nerves. The lead may be left in place for up to 4 weeks.
Also Check: Urinary Tract Infection Kidney Pain
Existing Treatments Other Than Technology Being Reviewed
Treatments for Urge Incontinence
Generally, there are 4 broad areas of treatment for urge incontinence: behaviour modification, drug therapy, interventional therapy , and surgery. Diapers or pads are used throughout treatment and may be used in conjunction with the treatments. Patients who are treated successfully may still require diapers, but to a lesser extent.
Behaviour modification therapies include diet modification , toileting assistance , bladder training or retraining , pelvic muscle rehabilitation , and biofeedback. Behaviour modification is sometimes overlooked as the first treatment option for patients with urge incontinence. In a study assessing the treatment of 372 patients with urge incontinence, drug therapy was the first-line treatment for 50% of the patients, and only 13% were treated with behaviour therapy first.
A Cochrane review by Haye-Smith et al. investigating behaviour therapy in people with urinary incontinence specifically focused on pelvic floor muscle exercises in women. They reported that pelvic floor exercises were effective to manage stress and mixed incontinence however, the evidence supporting or refuting the use of pelvic floor exercises in women with urge incontinence was unclear. Similar to the conclusions by Wallace et al., Hay-Smith et al. reported that the studies included in their review reported various outcomes with little consistency between studies.
How The Interstim Systems Work
With the InterStim systems, the implanted neurostimulator and lead electrically stimulate the sacral nerve. This is thought to normalize neural communication between the bladder and brain and between the bowel and brain.1,2 Unlike oral medications that target the muscular component of bladder control, the InterStim systems offer control of symptoms through direct modulation of the nerve activity.1,2
One key advantage of this therapy is that it can be tested for potential success prior to implantation. The evaluation provides an opportunity to find out whether adequate symptom reduction is achieved in as few as three to seven days. Complications can occur with the evaluation, including tissue damage, infection, and technical problems with the device. Patients should be instructed on operating the programmer and given precautions related to the evaluation.
Medtronic Bladder Control Therapy –
A video of how the InterStim II system electrically stimulates the sacral nerve for bladder control therapy. More information Less information
The most common adverse events experienced during clinical studies of patients with SNM included pain at implant sites, new pain, lead migration, infection, technical or device problems, adverse change in bowel or voiding function, and undesirable stimulation or sensations. Any of these may require additional surgery or cause return of symptoms.
Don’t Miss: What Can I Do To Prevent Urinary Tract Infections
Gene Testing For Stress Urinary Incontinence
An UpToDate review on Evaluation of women with urinary incontinence states that The risk of urinary incontinence, particularly urgency incontinence, may be higher in patients with a family history. One study found that the risk of incontinence was increased for both daughters and sisters of women with incontinence. Twin studies attribute a 35 to 55 % genetic contribution to urgency incontinence/overactive bladder but only 1.5 % for stress incontinence.
Furthermore, an UpToDate review on Urinary incontinence in men does not mention genetic testing as a management option.
For Many People Living With Incontinence Sacral Nerve Stimulation Has Delivered Life
The treatment has given sufferers genuine hope for the improvement of these debilitating conditions.
Neuromodulation is a treatment that delivers either electricity, drugs or magnetic impulses to nerves in an effort to change their activity.
Sacral nerve stimulation is a means of directly stimulating the third sacral nerve with an electrical current to alter/improve bladder and bowel function, and modulate pelvic pain.
Over the past 23 years, there have been many improvements with the technique of SNS. Symptoms SNS can treat:
Refractory urgency, urge incontinence
Pelvic pain
Faecal incontinence
Constipation
Urinary urgency, urge incontinence, enuresis and the closely related problem of faecal urgency and incontinence are the two most common reasons for considering SNS.
The cause of these conditions may be undetermined, familial, associated with various neurological injuries or disease states while bladder tumours, polyps or stones must be excluded before considering this treatment.
Almost all patients considering SNS will have had, and for various reasons failed, standard medical therapy such as attention to pelvic floor function and various medications, and as these conditions are often life-long, no treatment can guarantee a cure, but the improvements gained are often life-changing.
Since its inception, approximately 4500 patients have received this treatment in Australia with the number expected to increase as awareness and confidence in the procedure grows.
Read Also: What Is The Best Medicine For Urinary Tract Infection
Adjustable Retropubic Suburethral Sling For Stress Urinary Incontinence
In a single-center, prospective study, Leizour and associates evaluated the safety and effectiveness of the adjustable suburethral sling Remeex in the treatment of male SUI. Participants were patients treated for SUI after radical prostatectomy or transurethral resection of prostate. The severity of incontinence was evaluated by the number of pads used per day. Success rate, complications and number of adjustments were studied. From February 2011 to May 2015, Remeex was implanted in 25 patients. The average pre-operative number of pads used per day was 3.8 . Sling tension has been adjusted the day after surgery in all patients. Mean follow-up was 31 months . During follow-up, 6 patients did not need any re-adjustment and 15 patients had to be re-adjusted. One Remeex system had to be completely removed because of a sub-occlusive syndrome 3 patients had early infection requiring partial system removal . At the end of follow-up, 9 patients were cured , 9 patients were significantly improved and 7 patients were not improved 5 patients were waiting for a new re-adjustment. The authors concluded that in this short series of patients who had prostatic surgery, at mid-term follow-up, the placement of an adjustable suburethral sling was associated with an improvement or cure of UI symptoms in 2/3 of cases.
Reject Incontinence And Its Effect On Your Life With Dr Bechara Tabet Dr David Heiser And Dr Steven Ochs From Urology One
Are you in control of your urinary tract system, or is it controlling you? When youâre suffering from incontinence, youâre never in complete control. And when youâre not in control, youâre likely to experience frequent leaks and the need to change pads, pants, and your plans.
Incontinence is a natural condition that develops with age, because of a procedure, or due to a health condition. But just because your body can no longer stop urine from staying in your bladder, it doesnât mean that you have to accept it. Learn more about your incontinence and our approach to your care here.
If youâre unexpectedly releasing urine, schedule an appointment with Urology One. You will learn more about your condition, treatment options, including sacral nerve stimulation with InterStim®, and how we can bring you long-term relief.
You May Like: Treat Urinary Tract Infection Over The Counter
What I Need To Know About Sacral Nerve Stimulation
Sacral nerve stimulation is treatment for urinary retention without blockage, overactive bladder symptoms, and fecal incontinence. Overactive bladder symptoms include urinary urge incontinence and urinary frequency. Electrical impulses are sent directly to the sacral nerves to improve or restore bladder or bowel function. Sacral nerves are in your lower back. They control anus, rectum, and bladder functioning. SNS is done when medicine and behavior therapy do not help improve symptoms. Implantation of an SNS includes 2 stages. The first stage is a trial phase to see if SNS will improve your symptoms. The second stage involves implanting the stimulator.
Precautions Related To Patient Programming And Patient Control Devices
Battery depletion: Individuals with very low perception thresholds may perceive fluctuations in the stimulation intensity as the battery nears depletion and may have to increase or decrease the amplitude to maintain symptom control.
Patients should carry a control device at all times to be able to adjust and/or turn off the Interstim. Patients with model 3023 must carry the patient programmer if the magnet is disabled.
The control device may affect other implanted devices and should not be placed over other implanted devices.
The patient programmer should not be immersed in liquid or cleaned with bleach, nail polish remover, mineral oil, or other similar substances.
When the programmer is in use, flammable or explosive atmospheres should be avoided.
The magnet used with model 3023 should not be placed on or near a computer, computer monitor, magnetic storage disks or tapes, televisions, cell phones, electronic personal information managers, credit cards, or other items affected by magnetic fields.
Don’t Miss: How Does Someone Get A Urinary Tract Infection