Which Uti Antibiotics Are Resistant
High rates of antibiotic resistance have been seen with drugs in the penicillin class, such as amoxicillin and ampicillin, some sulfonamides like sulfamethoxazole and trimethoprim , and the fluoroquinolone antibiotics .
Antibiotic resistance can be specific to local patterns in the community. Tell your doctor if you have taken an antibiotic in the last 3 months or traveled out of the country. If needed, your doctor can perform a culture and sensitivity test to see which antibiotic might work best for your infection.
Keep taking your antibiotic even if you feel better and you think you don’t need your antibiotic anymore, unless your doctor tells you to stop. Only partially finishing your antibiotic may increase your risk of antibiotic resistance and your infection may return quickly.
What Type Of Bacteria Usually Cause Urinary Tract Infections
The most common bacterial cause of UTIs are E coli. These bacteria usually live harmlessly in the gut of healthy people but can cause problems if they get into the bladder or other parts of the urinary tract. Uncomplicated infection of the bladder, also called cystitis, is common and can be very painful.
Some strains of E. coli bacteria have begun to produce enzymes called extended-spectrum beta-lactamases . These can make the bacteria resistant to certain antibiotics, and so the bacteria continue to multiply and spread. This causes more severe infection which becomes much more difficult to treat. Another type of bacteria which often causes antibiotic resistant UTIs is ESBL klebsiella pneumoniae. You can read more about extended-spectrum beta-lactamase-producing bacteria here.
E. coli belongs to the Enterobacteriaceae family of Gram-negative bacteria. This family of bacteria also include klebsiella pneumoniae and enterobacter cloacae. The Enterobacteriaceae family can all cause UTIs and are often treated with the beta-lactam antibiotic, carbapenem, for which there are specific ESBL enzymes. The carbapenem resistant Enterobacteriaceae that have developed, have become a real risk to health as the main antibiotic becomes useless and their presence increases in hospitals and care settings.
Calculating The Theoretic Risk Of Therapy Failure
The theoretic risk of antibiotic failure depends on two factors the prevalence of the microbes in the patient population and the resistance rate of these microbes to the chosen antibiotic . We calculated the theoretical risk of therapy failure by multiplying the relative percentage each microbe was responsible for with the resistance rate for that antibiotic . We performed these calculations for each of the five most commonly isolated microbes E coli, E faecalis, K pneumoniae, P mirabilis, and P aeruginosa.
Also Check: Can Lower Back Pain Cause Urinary Incontinence
Many Factors Tied To Multidrug
A study conducted in France suggests human, animal, and environmental exposures may all be linked with the occurrence of community-acquired, multidrug-resistant urinary tract infections .
The findings on UTIs caused by extended-spectrum beta-lactamase -producing Escherichia coli were reported yesterday in JAMA Network Open.
While these multidrug-resistant UTIs have long been a problem in hospitals and other healthcare facilities where patients are routinely exposed to bacterial pathogens and antibiotics, the incidence of community-acquired ESBL-producing E coli UTIs has grown in recent years, with a variety of factors cited as potential culprits. ESBL-producing E coli is considered a growing public health threat because the ESBL enzyme confers resistance to multiple classes of antibiotics and makes common infections like UTIs difficult to treat.
The authors of the study say the findings highlight the importance of surveillance and mitigation strategies that take a One Health approach.
Nership Can Overcome Timing Challenges

When confronted with a painful UTI, patients are understandably eager to clear up their symptoms. Yet prescribing the most effective antibiotic requires laboratory testing that can take 3-4 days. This lag can lead to well-meaning doctors prescribing a broad-based antibiotic in hopes of providing quick relief.
To overcome this challenge, partnership between providers and patients is key. Patients should expect to leave a urine sample for testing, even if they receive a prescription antibiotic. If symptoms do not improve within 72 hours after starting the drug, they should contact their doctor to start a different medicationby that time, lab results likely will be available.
Working together, we can reduce the burdensome symptoms of UTI, lower treatment costs, and improve outcomes for all patients with this common condition.
You May Like: How Can You Get Rid Of A Urinary Tract Infection
Who Is At Risk From Antibiotic
Those at greatest risk of antibiotic resistant infections are often those with other underlying medical conditions, have weakened immune systems either due to illness or as a side-effect of current treatment. Those often affected have already been taking antibiotics or have been in hospital. Older people, such as those in care facilities or those undergoing catheterisation may also be affected by ongoing or recurrent resistant UTIs.
The biggest risk is that untreated or resistant infections can lead to kidney problems or even more serious conditions like sepsis . However, it is also very difficult living with the ongoing symptoms of recurring or antibiotic resistant UTIs.
Microbiologic Analysis And Susceptibility Testing
Urine cultures fulfilling the criteria for significant bacteriuria were included in the study. For Gram negative rods the automated method Vitek 2 was used. Appropriate antibiotics were selected for each bacterial species according to recommendations from the Norwegian Working Group on Antibiotics . Results were interpreted according to clinical breakpoints from NWGA which are based on those from The European Committee on Antimicrobial Susceptibility Testing EUCAST . Dip-agar isolates and Gram positive bacteria were tested by disk diffusion technique after the manufacturers recommendations. Resistance values were recorded either as susceptible , intermediate , or resistant .
Resistance data were extracted from the laboratorys database.
Recommended Reading: Urinary Tract Infections Utis Antibiotics
Antibiotic Warnings And Treatment Concerns
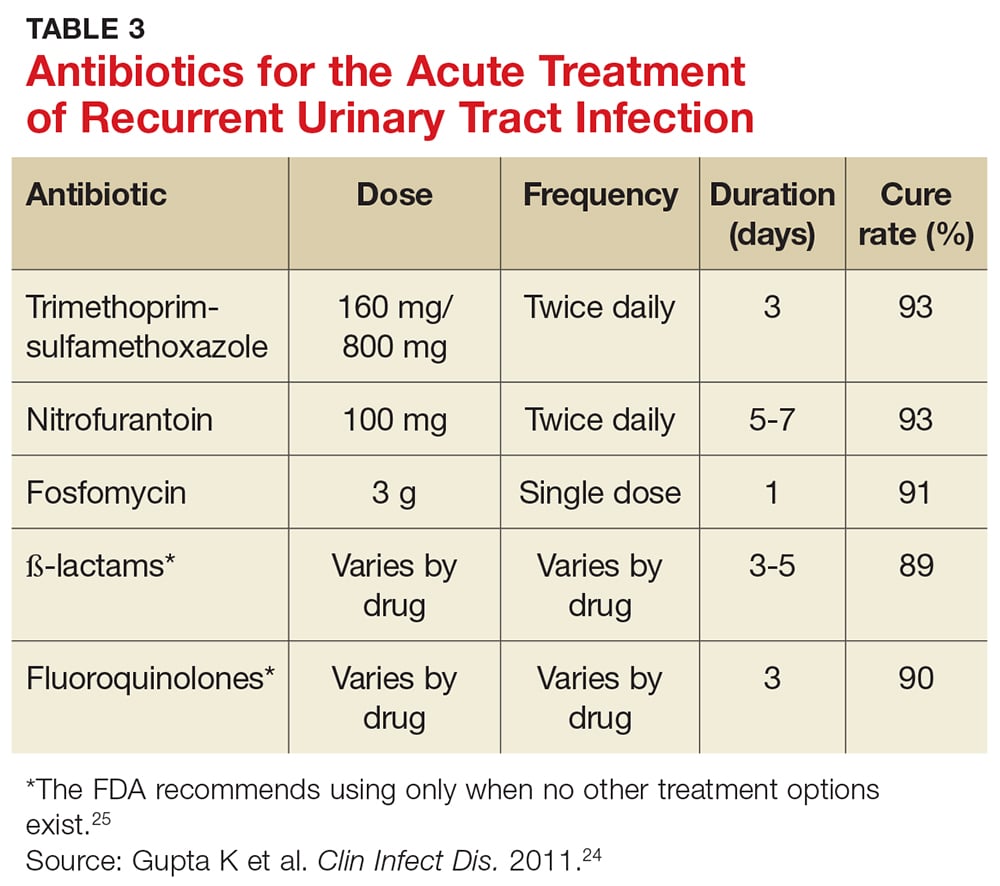
The most commonly prescribed antibiotics for uncomplicated UTIs are similar in efficacy. But its important to note that ampicillin, amoxicillin, and sulfonamides are no longer the drugs of choice for combatting UTIs because of the emergence of antibiotic resistance. In addition, amoxicillin and clavulanate has been shown in previous research to be significantly less effective than others when it comes to treating urinary tract infections.
Also, as noted above, the FDA advises against using fluoroquinolones for uncomplicated UTIs. These medicines should only be considered if no other treatment options are available. In some cases, such as a complicated UTI or kidney infection, a healthcare provider may decide that a fluoroquinolone medicine is the best option, notes the American Academy of Family Physicians.
For pregnant women, some common antibiotics, such as fluoroquinolones and tetracyclines, should not be prescribed because of possible toxic effects on the fetus. But oral nitrofurantoin and cephalexin are considered good antibiotic choices for pregnant women with asymptomatic bacteriuria and acute cystitis, according to past research.
Antibiotic Resistance Is Now Common In Urinary Tract Infections
The number of urinary tract infections caused by drug resistant bacteria is increasing, new data shows.
23 October 2017
The ‘English Surveillance Programme for Antimicrobial Utilisation and Resistance report says more than one million UTI samples were analysed in NHS laboratories across England last year , and that resistance was a common observation.
One in three of the samples analysed were found to be resistant to an antibiotic called trimethoprim, compared to 29.1% in 2015.
Trimethoprim was once the first choice treatment for UTIs before Public Health England recommended switching to a different antibiotic called nitrofurantoin. Only 3% of the UTI samples showed resistance to nitrofurantoin, the report says.
Inappropriate use of antibiotics, such as taking them for viral conditions like flu, or for mild infections that may clear-up without treatment is known to fuel resistance.
NICE recently updated its guidance for managing UTIs in children. New recommendations focus on using urine dipstick tests to identify whether antibiotic treatment is needed.
Professor Gillian Leng, deputy chief executive at NICE said:Antibiotic resistance is one of the greatest dangers to our health, which is why we must all work together to fight it.
Making sure that we use these medicines properly, only when they are really needed, is vital. And our guidance is here to help healthcare professionals navigate these sometimes difficult decisions.
Also Check: Are Probiotics Good For Urinary Tract
Take Antibiotics As Directed
If youre prescribed antibiotics, take them exactly as your doctor tells you to. That means no skipping doses or using leftover pills months later. Follow your doctors instructions for how long to take the pills for: if youre supposed to take them for two weeks, take them for two weeks, even if you start feeling better sooner.
An Ounce Of Prevention
Unfortunately, most UTIs are not completely preventable, and are caused by differences in the structure or function of the urinary tract and immune system. But there are things you can do to keep healthy. For example, stay hydrated to increase urine production and flush out unwanted bacterial intruders. Good hygiene is also important, but scrubbing away at delicate genital tissues can damage them and create portals for bacteria. Clean your genital area gently with mild soap and water. Postmenopausal women may benefit from vaginal estrogen cream. Finally, eating cranberries and urinating after having sex havent been proven to have major benefits, but arent likely to hurt, either.
Follow me on Twitter@lisa_xpond
About the Author
Lisa Bebell, MD, Contributor
You May Like: Home Remedy For Feline Urinary Tract Infection
Extended Data Fig 6 Model Performance On Test And Training Data
AUC for receiver operator characteristic for prediction of resistance based on demographics, sample history and purchase history, individually and in a complete model combining all feature sets. Each feature set was modeled using LR, and the complete model was modeled by both LR and GBDT. To identify overfitting, model performance on the testing data set was contrasted with model performance on the training data set . A low level of overfitting is seen for all drugs except trimethoprim, which showed no overfitting. See Supplementary Fig. for feature importance in GBDT models.
Extended Data Fig 8 Schematic Diagram Of Machine
A set of samples with features of demographics, sample resistance history and antibiotic purchase history labeled for resistance to each antibiotic k is used to train an antibiotic resistance prediction model . The model is applied to an SDET set of cases from the test period to calculate the probabilities of resistance to each antibiotic. In an unconstrained model the antibiotic with minimal probability for resistance is suggested. The calculated probabilities of resistance together with the respective prescriptions of the SDET set of cases are used to add a cost term. In a constrained drug prescription model, the antibiotic with the minimal cost-adjusted probability is suggested.
Read Also: How To Clean Out Urinary Tract
How Quickly Will The Infection Spread Is There Anything I Can Do To Stop It Getting Worse
The speed at which an infection spreads depends on many factors. This includes the type of bacteria causing the infection and how long they infection has been present for. The genetics of the bacteria involved and the health and habits of the person affected is also a factor. It remains important to maintain good hygiene and follow the advice of your doctor or clinical specialist. You should also let them know if you notice any changes in your condition. The biggest risk is that the infection is not treated quickly enough or effectively. This can also increase the risk of developing kidney infection, inflammation or urosepsis increases. When the bacteria spread from the urinary tract or bladder into the bloodstream, it is commonly called urosepsis, and can be very serious.
Resistant Uti Bacteria In Uninfected Women
In the new Clinical Infectious Diseases study, researchers tested stool samples from more than 1,000 healthy women who were free of UTI symptoms. The women were from the Puget Sound area of Washington.
The tests revealed that 8.8% of the women were carrying fluoroquinolone resistant strains of E. coli in their guts.
Doctors frequently prescribe fluoroquinolones for the treatment of UTIs. The researchers note that, although there have been efforts to limit the use of these antibiotics, resistant strains of bacteria are spreading widely.
In addition, the researchers found that most of the fluoroquinolone resistant E. coli bacteria also belonged to two widespread, multidrug resistant strains that are responsible for most hard-to-treat urinary and blood infections.
The researchers also tested urine samples that the women had given at the same times as the stool samples.
These tests revealed that more than one-third of the women with fluoroquinolone resistant E. coli gut bacteria also had E.coli in their urine. Of these, almost 77% had fluoroquinolone resistant strains that matched those of their stool samples.
Of the women, 45 also gave permission for the team to track their medical records. These showed that 7% of them went on to receive diagnoses of UTI some 3 months later.
Recommended Reading: Royal Canin Urinary So Dry Food
How Do I Know If My Particular Strain Of Uti Is Resistant To A Particular Drug
The only way is to get a urine culture. The lab results will identify the germ and what would be effective in treating the infection. But it can take several days to get the results.
Most patients want an immediate prescription so doctors usually make a best-guess determination of what drug will work given a patients symptoms and history.
The importance of history cannot be overstated if you have had a previous U.T.I., a previous resistant U.T.I., or have traveled outside the country, your history can help a doctor decide which drug to use.
Increasingly, experts tell us that you should ask for a culture when you go in for a U.T.I. treatment, even if you get an immediate prescription. The culture will allow a doctor to change the drug if the first one does not work.
That said, there is an important catch about when to do a urine culture. Often, it will show bacteria in the bladder even when an infection is not present. Some amount of bacteria is normal. The Infection Disease Society of America cautions doctors against doing cultures when symptoms of a U.T.I. are not present. The culture likely presence of bacteria can then lead to prescription of unnecessary antibiotics, contributing to the rise of resistance through overuse of the drugs.
Finally, some U.T.I.s, even when there are symptoms, can clear up on their own. This is one of many reasons to seek the care of an informed professional.
What You Need To Know About Resistant Urinary Tract Infections
U.T.I.s are one of the worlds most common infections, but many of the drugs used to treat them have become less effective as resistance to antibiotics grows.
-
Send any friend a story
As a subscriber, you have 10 gift articles to give each month. Anyone can read what you share.
Give this articleGive this articleGive this article
By Matt Richtel
Urinary tract infections, or U.T.I.s, are one of the worlds most common infections. Increasingly, they also are resistant to major drug treatments. Heres what you should know.
You May Like: Royal Canin Urinary So Feline Treats
What Is Colonisation And Biofilm
When people have had several UTIs, and several courses of antibiotics for a UTI, antibiotics may initially appear to work and symptoms often resolve for a while. However, the more resistant organisms are known to sometimes attach themselves to the bladder wall as well as forming colonies of resistant bacteria within other parts of the body such as the kidney.
These colonies of resistant bacteria can multiply in number over time, and become immune to the effect of the antibiotics. The bacteria become harder to eradicate, even when taking powerful antibiotics, as they form a biofilm. This is where the colonies of resistant bacteria form a protective layer around themselves, making it even more difficult for antibiotics to reach and kill them.
An antibiotic resistant UTI can then become a chronic condition and can often cause frequently recurring outbreaks of infection, with an increased risk of serious kidney infection and even sepsis.
Small Compounds Targeting Urease
Urease, an enzyme which catalyzes the hydrolysis of urea, is crucial in the pathogenesis of several uropathogenic bacteria such as P. mirabilis, Klebsiella sp., Pseudomonas sp. and Staphylococcus sp. . This enzyme leads to the alkalinization of the urine and the production of struvite and carbonate apatite that make up the major component of urinary stones . These conditions lead to the inflammation of the urogenital epithelia thus increasing the risk of catheter-associated biofilm formation that may contribute to pyelonephritis , mainly due to both bacterial and host cysteine protease .
The most studied inhibitors of urease are hydroxamic acids . These molecules have a high inhibitory activity against urease, by bonding to the two nickel ions in the urease active site . Initially, these molecules were used to treat UTIs by preventing urine alkalization . However, because of the growing evidence of side effects such as mutagenic power, they were progressively phased out .
Through similarly interacting with nickel ions in the urease active site, the phenyl phosphoramidates were found to have the highest inhibitory activity . Studies testing these molecules in an in vitro model and in a rat model found promising results. Since then, no in vivo studies or clinical trials have been developed, probably due to the poor hydrolytic stability of these molecules which leads to a very short half-life .
Don’t Miss: Dosage For Azo Urinary Tract Defense
Recurring Urinary Tract Infections Antibiotic Resistance And Acutis Reveal Uti
Most women who have experienced a urinary tract infection know the symptoms well a frequent urge to urinate yet pass little urine, cloudy and strong-smelling urine, a burning sensation when passing. 25%-30% of women who have had a UTI often suffer from a recurring UTI within six months of their first infection.
“Recurrent UTIs aren’t due to poor hygiene or something else that women have brought on themselves. Some women are just prone to UTIs,” says infectious diseases specialist Dr. Kalpana Gupta, a lecturer in medicine at Harvard Medical School.
Urinary tract infections are among the world’s most common infections, but many of the medications used to treat urinary tract infections, especially recurring ones, have become less effective as antibiotic resistance grows.
Patients suffering from recurring UTIs require accurate testing and rapid, high-quality results. Our urinary tract infection test – Acutis Reveal UTI – utilizes PCR-based testing methodology followed by antibiotic sensitivity testing information for enhanced accuracy and treatment insights.
Acutis Reveal UTIresults include AST information to assist practitioners in preventing potential overuse or inappropriate use of antibiotics that can lead toantibiotic resistance. Antibiotic sensitivity tests can help determine which antibiotic can most effectively treat a specific infection and provide insight into treatment for anantibiotic-resistant infection.