How Do I Do Kegel Exercises
Kegel exercises are a simple way to build strength in your pelvic floor muscles. These exercises are done by lifting, holding and then relaxing your pelvic floor muscles. You can find these muscles by stopping the flow of urine mid-stream while youre urinating. Only do this until you learn how to find the muscles stopping the flow of urine mid-stream isnt healthy over a long period of time.
When youre doing Kegel exercises, start small. Only hold it for a few second. Over time you can slowly work your way up to longer and longer stretches of holding the muscles tight.
Unlike other types of workouts, no one can tell when youre doing Kegel exercises. Aim to do several sets of Kegel exercises twice a day.
Management Strategies For Ui Among The Elderly With Dementia
It is often important to ask about UI in the presence of caregivers, as UI is frequently not reported voluntarily by the caregivers. Many of the elderly who are frail and demented have other comorbidities and the aetiologies for UI are often multiple. Even though UI cannot be cured, it can be managed and contained with appropriate continence aids to achieve a social/acceptable continence .
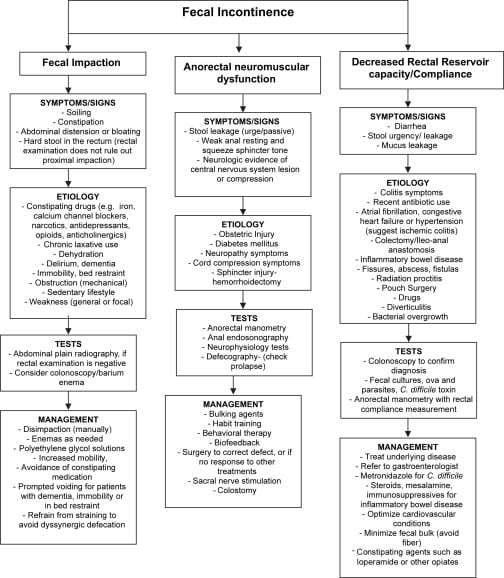
Figure 1: Summary of management of UI. View Figure 1
It is important to establish goals of treatment with the caregivers and the elderly with dementia. The goals include decrease in specific symptom burden, dryness or using less continence aids for protection, enable social activities to maintain/enhance quality of life, maintain the current place of residence and reduce caregiver burden .
From an elderly with dementia’s point of view, treatment options are rather limited because of the impaired cognitive function and pharmacological treatment may cause worsening of the cognitive function. Treatment options for UI consist of non-pharmacological means and pharmacological.
How Is Incontinence Treated
There are many different factors that your healthcare provider will consider when creating a treatment plan for your incontinence. The type of incontinence and the ways it affects your life are both big considerations. Your provider will also talk to you about the type of treatment you are most comfortable with. There are three main types of treatment you can explore for incontinence medications, lifestyle changes and surgery. Each option has pros and cons that your provider will discuss with you.
Medications to treat incontinence
There are quite a few medications that can reduce leakage. Some of these drugs stabilize the muscle contractions that cause problems with an overactive bladder. Other medications actually do the opposite thing relaxing muscles to allow your bladder to empty completely. Hormone replacement therapies can often involving replacing estrogen thats decreased during menopause may also help restore normal bladder function.
In many cases, medications can work very well to return normal function to the bladder. Your provider will carefully select a medication that matches your specific needs. Often, your provider will start you on a low dose of the medication and then increase it slowly. This is done to try and reduce your risks of side effects and to keep track of how well the medication is working to treat your incontinence.
Common medications that can be used to treat incontinence include:
Lifestyle changes to manage incontinence
You May Like: How To Treat Urinary Urgency
Behavioral Therapy: The First Treatment For Urinary Incontinence In The Elderly
After a diagnosis is made, behavioral therapy is often the first urinary incontinence treatment for the elderly. This may involve:
Learning to delay urination
You can do this by gradually lengthening the time between bathroom trips. One can also practice double voiding, which is when a person urinates, waits for a few minutes, and then urinates again. This teaches the person to drain their bladder more thoroughly.
Scheduled bathroom visits
This is often effective for people with mobility issues or neurological disorders, even if this means someone else is in charge of taking you to the restroom.
Pelvic floor muscle exercises
Called Kegels, these exercises strengthen the muscles that help regulate urination. Usually one needs to practice these a few times a day, every day. Learning how to contract the right muscles can be confusing, but your medical provider or this step-by-step guide to performing Kegel exercises can help.
Fluid and diet management
Although diet alone cant cure urinary incontinence, it can improve bladder control. Certain beverages like carbonated drinks and alcohol can cause your bladder stress. Even drinking coffee or tea while taking prescribed medication can aggravate it. Additional bladder irritants to avoid include milk, tea, honey, soda, and very spicy foods.
What Causes Urinary Incontinence In The Elderly
From not drinking enough water to childbirth to a health condition such as diabetes, there are many different reasons behind urinary incontinence.
The following health issues can cause urinary incontinence in both women and men:
- Multiple sclerosis
For men, prostate problems are a common cause of urinary incontinence.
Read Also: Natural Cure For Urinary Incontinence
When To Seek Medical Advice
See a GP if you have any type of urinary incontinence. Urinary incontinence is a common problem and you should not feel embarrassed talking to them about your symptoms.
This can also be the first step towards finding a way to effectively manage the problem.
The GP may also suggest you keep a diary in which you note how much fluid you drink and how often you have to urinate.
Find out about diagnosing urinary incontinence.
Management Of Urinary Incontinence In The Elderly
Management of urinary incontinence in the elderly is possible and can help seniors remain active.
While common in senior loved ones, urinary incontinence is a challenging condition to handle, impacting everyday life in a variety of ways and frequently leading to reduced self-confidence and assurance in addition to the limiting of enjoyable activities.
However, it is important to realize that urinary incontinence is not something that has to simply be accepted as an ordinary part of aging. Figuring out the root cause of the problem can result in a highly effective treatment option. Contributing factors to bladder control problems include:
- A urinary tract or vaginal infection
- Weakened or overactive bladder muscles
- Pelvic organ prolapse or weakened pelvic floor muscles
- Nerve damage from conditions such as Parkinsons disease, diabetes, or MS
- Enlarged prostate
- Health conditions which make it harder to get to the restroom in time, such as arthritis
An older adult going through difficulties with incontinence should visit with the doctor to talk about symptoms, medications, and medical background. She or he may recommend blood and urine tests as well as testing to figure out how effectively the bladder is emptying. Keeping a daily journal prior to the appointment may help, observing the times of day when urinating and when leaking urine.
When the reason behind the incontinence has been confirmed, treatment plans can include:
Read Also: Myasthenia Gravis And Urinary Incontinence
Medication For Incontinence In The Elderly
Medications are frequently used in combination with behavioral therapies. Here are some commonly prescribed options:
Anticholinergic or antispasmodic drugs
These are usually prescribed for urge incontinence. Examples include Vesicare®, Detrol LA®, Ditropan XL®, Oxytrol skin patch®, and Santura®. The most common side effect is dry mouth. Less common side effects include blurred vision, constipation, and mental confusion.
Antibiotics
These are prescribed when incontinence is caused by a urinary tract infection or an inflamed prostate gland.
H4) Tofranil® and Sudafed® These are used to treat stress urinary incontinence, and they work by tightening muscles around the bladder.
Basic Neurophysiology Of Micturition
The bladder is innervated by the autonomic nerves as well as the somatic nerves. The sympathetic innervation originates at T11-L2, supplying the bladder via the Hypogastric nerve. The parasympathetic nerves originate at S2-S4 and innervate the bladder via the Pelvic and Pudendal nerves.
The sensation of bladder fullness as it fills ascends via the spinal cord to be conveyed to the Pontine Micturition Centre, which promotes micturition via the parasympathetic supply to the urinary bladder. However, micturition may not be appropriate at all times. The central nervous system determines the “correct timing” of micturition, taking into account the social and behavioural part of micturition. Micturition is coordinated and triggered through simultaneous activities of the bladder contraction with relaxation of the urethral sphincters via the somatic and autonomic nerves.
In addition to the complex neuroanatomical and physiological reflexes to maintain continence, there are other faculties needed to maintain continence. An intact cognition is important to perceive the sensation of bladder fullness with the ability to postpone micturition after the first sensation, motivation and desire to pass urine, sufficient mobility and coordination to reach the toilet with hand dexterity to manipulate clothing items in order to do so. In addition, the ability to locate the toilet with clear direction and access also contribute to continence .
Don’t Miss: Can Hep C Cause Urinary Tract Infection
Etiology And Risk Factors
Multiple factors, including age-related physiological changes, may result in or contribute to the various syndromes of UI. Both genitourinary and non-genitourinary factors may contribute to incontinence in aging patients. Age-related functional changes in the urinary tract may contribute to UI.32 In women, risk factors for these genitourinary changes include multiple or complex vaginal deliveries, high infant birth weight, a history of hysterectomy, and physiological changes related to the transition to postmenopause. Smoking, a high body mass index, and constipation are also associated with an increased risk of UI.3337
Pathophysiological causes of UI include lesions in higher micturition centers, in the sacral spinal cord, and in other neurological areas as well. UI may also be associated with numerous comorbidities, such as Parkinsons disease, Alzheimers disease, cerebrovascular disease, diabetes, hypertension, obstructive sleep apnea, and normal-pressure hydrocephalus. Functional factors, including mobility and dexterity, along with reaction time and lack of access to a bathroom facility, may also contribute to UI.3337
Urinary Incontinence In Older Adults
Urinary incontinence means a person leaks urine by accident. While it can happen to anyone, urinary incontinence, also known as overactive bladder, is more common in older people, especially women. Bladder control issues can be embarrassing and cause people to avoid their normal activities. But incontinence can often be stopped or controlled.
What happens in the body to cause bladder control problems? Located in the lower abdomen, the bladder is a hollow organ that is part of the urinary system, which also includes the kidneys, ureters, and urethra. During urination, muscles in the bladder tighten to move urine into the tube-shaped urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder dont work the way they should, urine can leak, resulting in urinary incontinence.
Incontinence can happen for many reasons, including urinary tract infections, vaginal infection or irritation, or constipation. Some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
- Weak bladder or pelvic floor muscles
- Overactive bladder muscles
- Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinsons disease
- Diseases such as arthritis that may make it difficult to get to the bathroom in time
Most incontinence in men is related to the prostate gland. Male incontinence may be caused by:
You May Like: Too Many Urinary Tract Infections
Am I At A Higher Risk Of Incontinence At An Older Age
Your body constantly changes throughout your life. As you age, the muscles that support your pelvic organs can weaken. This means that your bladder and urethra have less support often leading to urine leakage. Your risk for developing incontinence as you age might be higher if you have a chronic health condition, have given birth to children, went through menopause, have an enlarged prostate or have had prostate cancer surgery. Its important to talk to your healthcare provider over time about the risks of incontinence and ways you can manage it without interference to your daily life.
Incontinence In Older Adults: The Role Of The Geriatric Multidisciplinary Team
Urinary and fecal incontinence are very common in the geriatric population, yet many patients and health care practitioners wrongly consider incontinence a normal part of aging.
Older adults require an incontinence assessment that includes a review of physical, psychological, and social health. Functional status, quality of life, and goals of care must also be considered. Quality of life for older patients can be improved with the help of a nurse continence advisor , a pelvic floor physiotherapist, a geriatrician, and other health professionals skilled in the assessment, diagnosis, and management of urinary and fecal incontinence.
The nurse continence advisorThe nurse continence advisor is a registered nurse who has recognized education, training, and certification in continence management. The NCA focuses on conservative and holistic strategies for managing incontinence and related symptoms, including urinary urgency, frequency, and nocturia, and fecal incontinence and constipation. This nursing specialty was developed in Great Britain in the 1970s in response to long wait lists to see urological specialists, and was introduced in Canada in 1995 by the Ontario Ministry of Health.
This article has been peer reviewed.
Recommended Reading: Herbs For Urinary Tract Health
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association /International Continence Society joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2010 21:526. This consensus statement provides consistent terminology to enable clinicians to communicate more effectively regarding care of patients with UI.
How A Health Professional Can Help
The first health professional that youre likely to talk to about incontinence is your primary care provider, but they may refer you to another physician or professional who can better help. Urologists and gynecologists are surgeons who see men and women for incontinence, and nurse continence advisors can run specialized interprofessional clinics.
Diagnosing the cause of incontinence
What your doctor will ask about: The treatment of incontinence depends on the cause of the symptoms, which your doctor will evaluate by asking questions, doing a physical examination, and probably order a few preliminary investigations.
Your doctor will review your personal medical history, especially any history of prostate surgery for men, and for women, the history of any pregnancies and number and types of births. Lifestyle issues like smoking, alcohol intake, caffeine consumption, exercise , and body weight are likely to come up.
A careful review of the patterns of incontinence will help to determine the cause of urine loss.
To review, three common patterns of urinary incontinence are:
- Stress: if you lose urine when doing certain activities,
- Overflow: you lose urine all the time in a dribble,
- Urge: feeling an urgent need to get to the toilet that you sometimes cant meet,
In older adults, its common for there to be a mixture of more than one pattern .
Your doctor will want to know:
The physical examination
Tests
Recommended Reading: Medicine To Stop Urinary Burning
How To Deal With Elderly Incontinence
Your loved one may feel embarrassed by their accidents and avoid scheduling a doctors appointment. They may be using absorbent pads or protective underwear to help, but urinary incontinence is very treatable with medical assistance.
They may also hold off because theyre unsure what kind of doctor to see. A primary care doctor, geriatrician, nurse practitioner, or urinary specialist are viable options. If your loved one feels comfortable with their primary care doctor, its generally good to start there.
Women can also find a urogynecologist, while men can visit a urologist.
Is Incontinence More Common In Women
Incontinence is much more commonly seen in women than in men. A large part of this is because of pregnancy, childbirth and menopause. Each of these events in a womans life can lead to bladder control issues. Pregnancy can be a short-term cause of incontinence and the bladder control issues typically get better after the baby is born. Some women experience incontinence after delivery because of the strain childbirth takes on the pelvic floor muscles. When these muscles are weakened, youre more likely to experience leakage issues. Menopause causes your body to go through a lot of change. Your hormones change during menopause and this can alter your bladder control.
Men can also experience incontinence, but it isnt as common as it is in women.
Don’t Miss: Natural Supplements For Urinary Incontinence
How Is Incontinence Diagnosed
Often, the diagnosis process for incontinence will start with a conversation with your healthcare provider about your medical history and bladder control issues. Your provider might ask you questions like:
- How often do you urinate?
- Do you leak urine between trips to the toilet, how often does this happen and how much urine do you leak each time?
- How long have you been experiencing incontinence?
These questions can help your provider figure out a pattern with your leakage, which often points to a specific type of incontinence. When your provider is asking about your medical history, its important to list all of your medications because some medications can cause incontinence. Your provider will also ask about any past pregnancies and the details around each delivery.
There are also several specific tests that your provider might do to diagnose incontinence, including:
While at home, your provider might recommend you keep track of any leakage in a journal for a few days. By writing down how often you experience incontinence issues over the span of a few days, your provider might be able to identify a pattern. This can really help in the diagnosis process. Make sure to write down how often you need to urinate, how much you are able to go each time, if you leak between trips to the bathroom and any activities you might be doing when you leak urine. Youll then bring this journal with you to your appointment and talk about it with your provider.