Extrusion Into The Urinary Tract
Complications and symptoms include haematuria, recurrent UTIs, stone formation,fistula, urgency and voiding difficulty. It is important to inform the patientthat urinary symptoms might not improve, and new ones might appear. Likelihoodof developing SUI is about 1356%,34 with around 36% requiring another procedure for SUI in studies notlimited to extrusion as only criteria for mesh excision.35 The only study reporting data exclusively for mesh excision found 759%SUI after surgery but follow up is for less than 1year.36 There is a risk of developing a urinary fistula between the urethra andthe vagina or bladder and vagina.
Mesh in the urinary tract, in general, must always be removed as it is a nidusfor infection and stone formation. The least radical option is endoscopic lysisof the tape with laser or bipolar resection, which might allow the mesh toretract and facilitate a vaginal approach.37 Mesh excision, at the same time or as a second stage, will preventfurther extrusions. Complete excision of mesh with urinary reconstruction can bedone either through a vaginal, abdominal or minimally invasive approach.
Treatment for recurrent SUI, with an autologous fascial sling or colposuspension can be considered at the sametime of removal if there was SUI prior to mesh removal or as a possible secondprocedure if SUI recurs after mesh removal.
Complication Rates By Type Of Sling
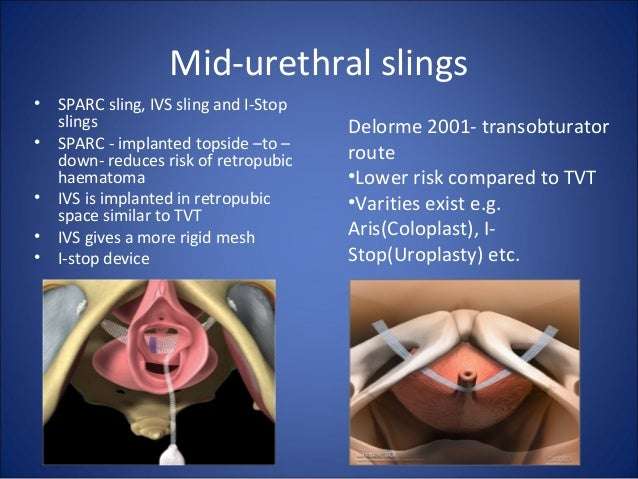
Before undergoing bladder sling surgery, women should ask their doctors about the technique they plan to use. Complication rates may vary depending on the type of mesh sling and technique.
A 2010 study of bladder sling procedures by Z. Chen and colleagues published in Urologia analyzed the outcomes of 187 women who received bladder slings to treat stress urinary incontinence. Authors found that transobturator vaginal tape inside-out and transobturator vaginal tape out-inside are simpler techniques with fewer complications compared to tension-free vaginal tape .
Women who used TVT had an average hospital stay of five days versus about two days for the TOT group.
The complication rate in the study was:
- 15.6 percent for tension-free vaginal tape
- 9.20 percent for transobturator vaginal tape inside-out
- 8.90 percent for transobturator vaginal tape out-inside
Complications from the procedures included discomfort with urinating, bleeding outside blood vessels and dysfunction of lower limbs. TVT was the only procedure associated with bladder perforation. Despite the complication rate, doctors found the slings safe.
The three tension-free urethral suspension techniques have similar efficacy, all of them are safe and effective procedures for the treatment of female SUI, authors wrote.
What Pelvic Floor Surgeries Use Mesh
It is important to note that the FDA has only stopped the sale and distribution of devices containing mesh used for the transvaginal repair of pelvic organ prolapse.
Two common pelvic floor surgeries that use mesh and are not affected by the FDA announcement are as follows:
- Transabdominal mesh to treat pelvic organ prolapse: This minimally invasive surgery is done by making a small incision in the abdomen or laparoscopically and inserting the mesh to support organs. This technique has existed for more than 30 years and is well studied and safe. Women should not be afraid of this, Dr. Harmanli says.
- Midurethral sling procedure: This surgery is the most common one used to treat stress urinary incontinence. A surgeon makes three small incisions and places a narrow strip of synthetic mesh under the urethra to lift and support it along with the neck of the bladder. This is the safest and least complicated procedure a woman can have for urinary incontinence, Dr. Harmanli says. There are approximately 20 years of high-quality data supporting this surgery. The risks are very minimal, and when there is a complication, it can be corrected with another surgery, but that is hardly ever needed.
Recommended Reading: What Do You Treat A Urinary Tract Infection With
Whats The Treatment For Vaginal Mesh Complications
We use antibiotics to treat the symptoms of infection, which may include oral medications or antibiotics delivered via intravenous infusion if the infection is severe. Otherwise, the most effective treatment typically requires surgical removal of the mesh and repair of the damaged tissue.
Its a delicate procedure that requires significant surgical skill and expertise. Removal of the mesh can be especially difficult because healthy tissue is often woven through the failing mesh, which must be carefully extracted to prevent further damage. Its also hard to determine the extent of tissue damage until surgery is underway, which can complicate the surgery further..
Depending on the extent and type of pelvic floor disorder youre experiencing, Dr. Kohli may recommend alternative surgical methods or other treatment strategies to help repair and strengthen the muscles of your pelvic floor.
If youre at risk for vaginal mesh surgery complications, schedule an appointment today with Dr. Kohli at Boston Urogyn. You can rely on his skill and expertise as a nationally and internationally respected pelvic reconstructive specialist.
You Might Also Enjoy…
What Are The Recommendations For Me If I Have Undergone Pelvic Reconstructive Surgery
You should follow up with routine check-ups and pelvic examinations each year. Let your healthcare provider know if you have symptoms such as vaginal bleeding or discharge, pelvic or groin pain, or pain during sexual intercourse. Tell your doctor about any surgical mesh implants if you plan to have surgery to treat a related condition or another type of operation. Talk to your provider if you have any questions or concerns.
Recommended Reading: Urinary Tract Infection And Bv
What Kind Of Surgery Is Effective For Female Urinary Incontinence
If you have stress incontinence, the 3 surgical options are usually colposuspension, sling surgery and vaginal mesh surgery. All 3 are known to effectively treat some women. But they dont help everyone, and its not possible to say for certain whether a particular surgery will be better for you.
Some women also get problems called complications after these types of surgery. These can include problems emptying your bladder fully, needing to pee urgently, or damage to your bladder or bowel. Generally, studies show that about 1 to 10 in 100 women get these problems .
In most cases, it isnt possible to say if 1 type of surgery is more likely to cause complications. For example, research suggests that
If you have urge incontinence, surgery is less likely to be effective, and procedures such as nerve stimulation or botox injections are more commonly recommended . Surgery is usually only considered in rare cases, if other treatments havent worked.
Whatever type of surgery or procedure is recommended for you, you should always discuss the risks and benefits with your doctor. Remember, its important that you make a choice thats right for your personal circumstances and this may mean not having surgery at all. Your doctor will be able to help you make a decision.
When Did Mesh Start Appearing In Pelvic Floor Surgery
Polypropylene mesh has been used for abdominal hernias since the 1950s. Historically, pelvic organ prolapse was repaired with native tissue, or attaching the prolapsed organ to a surrounding ligament or muscle with stitches. Although this is still a good option for many women, some women dont have enoughor strong enoughnative tissue, Dr. Rickey explains. Also, this technique is not always effective long-term, Dr. Harmanli notes.
So, in the 1970s, gynecologic and urologic surgeons began to experiment with mesh, cutting it themselves and inserting it through abdominal incisions. In the 1990s, a minimally invasive approachmaking an incision in the vagina to insert the mesh in an effort to shorten recovery timewas developed.
Meanwhile, the FDA approved the first pelvic mesh for stress urinary incontinence in 1996. In 2002, the first mesh for transvaginal repair of pelvic organ prolapse was approved. It was around that time when manufacturers began marketing kits that included surgical tools and mesh for transvaginal prolapse procedures, the first of which received FDA clearance in 2002.
Read Also: Enlarged Prostate And Urinary Incontinence
Less Commonly Used Treatments For Stress Incontinence
Urethral bulking
Urethral bulking is a procedure where a man-made bulking material is injected underneath the lining of your urethra and into the muscle at the neck of your bladder to prevent leaks.
Key things to know about urethral bulking:
- it can be an option if surgical treatment isnt right for you
- no cuts are made, its usually done under
What Should I Do After My Surgery To Treat Stress Urinary Incontinence
- Continue with annual check-ups and follow-up care, notifying your health care provider if complications develop, such as persistent vaginal bleeding or discharge, pelvic or groin pain, or pain during sexual intercourse. There is no need to take additional action if you are satisfied with your surgery and are not having complications or symptoms.
- If you have complications or other symptoms:
- Discuss complications and treatment options with your health care provider. Only your health care provider can give you personalized medical advice.
- Consider getting a second opinion from a surgeon who specializes in female pelvic reconstruction if you are not satisfied with your discussion with your health care provider.
Don’t Miss: Over The Counter Urinary Tract Infection Remedy
Data Preparation & Cleaning
Episodes were removed which were exact duplicates , Supplementary Table S1) and for patients with: an admission not coded as female age missing or under 18 years an invalid or missing admission method a missing admission date episodes after a reported date of death.
In this study we define insertion to mean the introduction of a mesh for the treatment of SUI, repair to mean a further procedure on a previously inserted mesh renewal to mean a procedure to remove a previously inserted mesh and to replace it with a new mesh and removal to mean the complete or partial removal of a previously inserted mesh. The OPCS-4 codes which correspond to each of these definitions are given in Supplementary Table S2.
In HES a spell is defined as one or more contiguous episodes within the same hospital admission. The index spell for each patient was defined as the earliest admission within the study period including one or more procedure codes for surgical mesh insertion excluding procedure codes indicating pelvic organ prolapse surgery , mesh repair, removal, renewal or subsequent mesh insertion20. Full details of codes and combinations used in this study are listed in Supplementary Tables S1 and S2.
Index spells without a coded diagnosis of incontinence or without an implied diagnosis of incontinence were excluded from analysis. Remaining eligible index spells were assumed to be first-time surgical mesh insertions for SUI.
The Main Benefits Of Using Mesh Instead Of Human Tissue Are
- mesh slings are faster and easier to place
- less time is spent in surgery
- incisions are smaller
- so healing is faster than if the sling was made from your own tissue.
- Mesh slings have been used to treat SUI for over 15 years. About 8 out of 10 women have no leaking or are drier after this procedure. As with any surgery, there can be problems or complications for some patients.
Mesh exposure in the vagina is one problem that can affect about 3 percent or 3 in 100 women after a mesh sling. This is when a piece of the mesh is not completely covered by the vaginal wall after healing.
A small edge of the mesh can be felt by the patient or their partner as a screen or gritty patch in the vagina. This can usually be fixed with a minor procedure to trim and cover the mesh. If the exposed mesh is not causing the patient any problems, it can be safe to leave untreated, and repair if new problems develop.
Mesh exposure is more common in patients that have thin delicate vaginal tissue from low estrogen. You may be advised to use estrogen vaginal cream before or after surgery.Rarely, the mesh causes painful scar tissue, erosion, or damage to the bladder or urethra. Some problems, especially pain are not able to be fixed with surgery.
There are three main types of mesh sling procedure: mini sling, retropubic, and transobturator. Each way of placing the mesh has its own risks and benefits.
Also Check: Lemon Juice And Baking Soda For Urinary Tract Infection
Fda Orders Mesh Manufacturers To Stop Selling Devices For Transvaginal Repair Of Pelvic Organ Prolapse
On April 16, 2019, after reviewing their premarket approval applications, the FDA ordered all manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling and distributing their products immediately. The FDA determined that the manufacturers, Boston Scientific and Coloplast, did not demonstrate reasonable assurance of safety and effectiveness for these devices, which is the premarket standard that now applies to transvaginal mesh for pelvic organ prolapse since the agency reclassified them into class III in 2016. For details, see the press release: FDA takes action to protect womens health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices. Following the FDA order in April 2019, the manufacturers withdrew these devices from the market.
People who received transvaginal mesh for the surgical repair of pelvic organ prolapse should continue with their annual and other routine check-ups and follow-up care. There is no need to take additional action if you are satisfied with your surgery and are not having any complications or symptoms.
You should notify your health care provider if you have complications or symptoms, including persistent vaginal bleeding or discharge, pelvic or groin pain, or pain with sex. You should also let your health care provider know if you have surgical mesh, especially if you plan to have another surgery or other medical procedures.
How Is Surgical Mesh Used To Repair Pelvic Organ Prolapse And Stress Urinary Incontinence
Surgical mesh can be permanently implanted to reinforce the vaginal wall for POP repair, or support the urethra or bladder neck for the repair of SUI.
There are three main surgical procedures performed using surgical mesh:
- Transvaginal insertion of mesh to treat POP.
- Transabdominal insertion of mesh to treat POP.
- Mesh sling to treat SUI: A multi-incision sling procedure may be performed in which three incisions are made. In the retropubic procedure, two very small incisions are made above the pubic bone and a third incision is made in the vagina. In the transobturator procedure, two very small incisions are made in the groin and thigh and one is made in the vagina. A mini-sling procedure, in which a shorter piece of surgical mesh is inserted, requires only one incision.
POP can also be repaired without surgical mesh. In that case, the incisions are usually made in the vagina, and they are closed with sutures only. Surgeries in which mesh slings are used have been successful in most cases and in about 70% to 80% of cases within one year following surgery.
SUI may also be surgically treated without surgical mesh. The surgeon can harvest a piece of your own muscle fascia to use in the shape of a sling to reestablish support of the bladder and urethra. In that case, fascia may be taken from your abdominal muscles through a C-section âbikiniâ incision, or from your leg muscles with an incision on the inner thigh.
Read Also: Mckesson Disposable Urinary Leg Bag
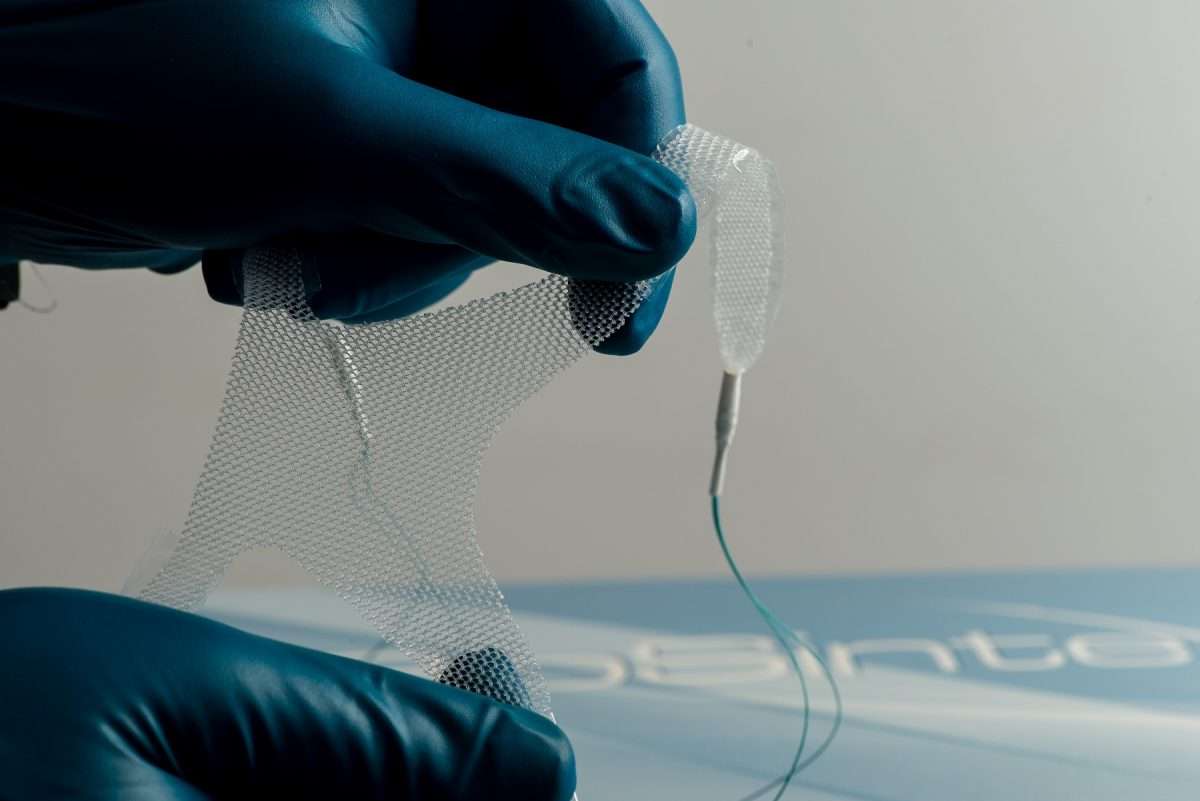
What Is Surgical Mesh
Surgical mesh is a screen-like material that is used as a reinforcement for tissue or bone. It can be made of synthetic polymers or biopolymers.
Materials used for surgical mesh include:
- Non-absorbable synthetic polymers .
- Absorbable synthetic polymers .
- Biologic .
- Composite .
Most surgical mesh devices used for female pelvic reconstructive surgery are made of non-absorbable synthetic polypropylene.
What Are The Symptoms Of Vaginal Mesh Complications
Symptoms of vaginal mesh complications may occur within weeks or months of the initial surgery and can include:
- Abnormal vaginal discharge and pain that may indicate an infection
- Pain with sexual intercourse, which your partner may also experience due to encountering loosening vaginal mesh material
- Vaginal bleeding that isnt related to your menstrual cycle
- Persistent pelvic pain
- Worsening incontinence, discomfort with urination, and other urinary symptoms
Infections related to vaginal mesh complications can quickly worsen and require prompt medical treatment. If you develop any of these symptoms following transvaginal mesh surgery, its important that you see your doctor as soon as possible.
Also Check: Can Weight Gain Cause Urinary Incontinence
Complications Of Vaginal Mesh Slings For Incontinence
Surgery that uses a synthetic mesh is the most common operation done to correct urinary stress incontinence in women, but may lead to complications or failure. Dr. Blaivas is an expert on reconstructive surgery for patients with significant mesh complications. He has published the largest series of reports in the world on women who have undergone urethral reconstructiona procedure that can help patients whose urethras were damaged by mesh surgeryand the largest series on treating urinary fistulas after mesh sling complications.
Mesh complications may cause new symptoms that were not present before the surgery. They may include:
- Difficulty urinating or inability to urinate at all due to a blockage by the sling
- Urinating too often and having to rush to the bathroom
- Urinary urge incontinence
- Recurring urinary tract infections
- Pain
- Vaginal discharge or bleeding
- Bladder stones
- Ureteral obstruction
If the bladder muscle is too weak, you may not be able to urinate normally even if there is no blockage from the sling. The best treatment for this is for you to learn to insert a catheter to empty the bladder. It sounds gruesome, but its not, and just about everybody can do it without difficulty. Fortunately, this condition improves in most people within a month or so and then the catheter is no longer needed.