What Is Stress Incontinence
Stress incontinence indicates a problem with the urethra or the valve that closes the bladder. Women will leak from the bladder when they cough, laugh or sneeze, or even change positions. This type of incontinence is usually related to the effects of childbirth or menopause that have weakened the pelvic support for the urethra.
Sometimes this type of incontinence can be combined with urge incontinence. Current research has not proven that hormone therapy improves incontinence conditions in any significant way.
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance
Crean-Tate KK, Faubion SS, Pederson HJ, Vencill JA, Batur P. Management of genitourinary syndrome of menopause in female cancer patients: a focus on vaginal hormonal therapy. Am J Obstet Gynecol. 2020 222:10313.
Blakeman PJ, Hilton P, Bulmer JN. Cellular proliferation in the female lower urinary tract with reference to oestrogen status. BJOG: An International Journal of Obstetrics & Gynaecology. 2001 108:8136.
Robinson D, Cardozo LD. The role of estrogens in female lower urinary tract dysfunction. Urology. 2003 Oct 1 62:4551.
Labrie F, Archer DF, Martel C, Vaillancourt M, Montesino M. Combined data of intravaginal prasterone against vulvovaginal atrophy of menopause. Menopause. 2017 24:124656.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in postmenopausal women. Cochrane Database of Systematic Reviews . 2012 Available from: .
Matarazzo MG, Caruso S, Giunta G, Valenti G, Sarpietro G, Cianci A. Does vaginal estriol make urodynamic changes in women with overactive bladder syndrome and genitourinary syndrome of menopause? Eur J Obstet Gynecol Reprod Biol. 2018 222:759.
Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011 186:5404.
Urinalysis And Bacterial Titers
Urine specimens from infected mice were collected at 0 to 14 days postinfection and serially diluted in PBS 5 l of each dilution was spotted onto LB plates six times as described previously . Bacterial titers were calculated as CFU/ml of urine. Urine sediments were obtained by cyto-centrifuging 50 l of a 1:5 dilution of the urine onto poly-l-lysine-coated glass slides, which were then stained for inflammatory scoring as described previously .
Also Check: What Are Symptoms Of Urinary Tract Infection In Females
Treating A Urinary Tract Infection
Most urinary tract infections can be treated quickly and easily with antibiotics, and fortunately, symptoms usually disappear within two days. When taking antibiotics, its important to take all of the doses prescribed, even if you are feeling better before you run out of your medication. Failing to take the entire prescription as recommended could result in a relapse of the infection.
Systemic HT may reduce the urinary symptoms of urgency, frequency, nocturia, and painful urination, but there is continuing debate about the effectiveness of systemic HT in treating urogenital atrophy.
Local estrogen, applied externally, is helpful in relieving the symptoms of urinary urgency, frequency, and stress incontinence, and can also help prevent urogenital atrophy and the recurrence of urinary tract infections.
The most common treatment for vaginal atrophy symptoms is low-dose vaginal estrogen level replacement, utilizing creams, tablets or vaginal rings.
However, some women are not able to have HT for any menopausal urinary symptoms such as women with breast cancer. For symptoms of vaginal atrophy, they can use vaginal moisturizers for normal relief and vaginal lubricants to relieve dryness prior to intercourse.
Upper urinary tract infections that affect the kidneys are much more serious and usually require a stay in the hospital. Your antibiotics may be administered intravenously while medical professionals monitor your health.
How To Increase Estrogen
Once you have established low estrogen levels, your physician might prescribe you hormones that can be taken orally, as well as a topical estrogen. Given the effects of estrogen on your vaginal flora, no wonder there are more and more studies demonstrating that estrogen treatment delivered vaginally may help prevent repeat urinary tract infections.
I suggest you also find out what causes your low estrogen levels and try to fix the core issue, if possible. You can do a lot by changing your lifestyle and diet to increase estrogen levels and using bio-identical estrogen products, but that is a topic for another post.
If you have an older female relative who suffers from frequent urinary tract infections , please share this information with her and her doctor. As you know, with the current state of medicine, physicians are more likely to play it safe and prescribe preventive doses of antibiotics to keep bacteria at bay. However, this approach builds up antibiotic resistance and has various side effects.
Check out other ways to prevent UTI naturally:
Read Also: Can Urinary Incontinence Cause Uti
Biofilm Formation And Endotoxin Release
We continued by investigating the effects of estradiol on biofilm formation and endotoxin release. The biofilm formation was significantly increased by 5 pg/ml estradiol compared with unstimulated CFT073 after 24 h. The higher concentrations of estradiol did not differ from unstimulated CFT073 in their ability to induce biofilm formation . When looking at endotoxin levels, we found no significant changes induced by estradiol compared with unstimulated CFT073 .
Figure 2. Biofilm formation and endotoxin release in the presence or absence of estradiol after 24 h. Data are presented as mean ± SEM of n = 3 independent experiments. The asterisk distinguishes statistical significance: *p< 0.05 vs. unstimulated CFT073.
The Pattern Of Incontinence Is Often Mixed
Symptoms of overactive bladder include frequency and nocturia . Some women also feel they need to pass urine, having only just done so due to over activity of the bladder muscle.
Recurrent urinary tract infections
UTIs can affect women of all ages, but this problem increases with age as a result of estrogen deficiency.
Management of urinary problems
Local estrogen
Local estrogen replacement therapy has been shown to alleviate urgency, urge incontinence, frequency, nocturia, dysuria and also to reduce urine infections.
Genuine Stress Incontinence would not appear to be helped by estrogen alone, but it does seem to improve the action of other treatments currently used.
The newer treatments including Ospemifene, DHEA and laser therapy may all have a beneficial effect on bladder problems.
Pelvic floor exercises
These can strengthen the pelvic floor reducing the risk of uterovaginal prolapse. Many women have learnt these techniques from childbirth, but it is well worth revisiting them.
Pelvic-floor physiotherapists are specialists in this field and are able to fully assess and monitor a womans pelvic floor function and teach appropriate techniques to strengthen it and retrain the bladder. They often use devices to help women perform appropriate exercises, such as weighted vaginal cones, or vaginal trainers. Your practice nurse or GP should be able to refer you to a specialist pelvic floor physiotherapist.
Surgery
Recommended Reading: Hills Feline C D Urinary Stress
Pelvic Floor Changes And Prolapse
The muscles and ligaments of the pelvic floor are all estrogen-sensitive, and changes in collagen, due to estrogen deficiency can have a profound effect on the support mechanisms of the pelvic floor.
The protective covering of the clitoris may be affected by changes in the urogenital tissue quality. The clitoris can become exposed and hypersensitive or buried underneath the fused labia minora.
What Is It Like Living With Vaginal Atrophy
Vaginal atrophy can seriously affect your quality of not just your sex life, but life in general. The pain, dryness, burning/itching, spotting, bleeding, urinary problems, UTIs and discharge can make you very uncomfortable and interfere with your daily living. One in four women report that vaginal atrophy has had a negative impact on other areas of their lives including their sleep, sexual health and general happiness.
Read Also: Itching In Urinary Tract Female
Estrogen A New Weapon Against Urinary Tract Infection In Menopause
Estrogen stimulates the production of the body’s own antibiotic and strengthens the cells in the urinary tract, according to a new study from Karolinska Institutet. The results, which are published in the scientific journal Science Translational Medicine, show that estrogen supplements may help menopausal women to ward off recurrent urinary tract infections.
Urinary tract infections are among the most common diseases, affecting over half of all women at some point in life and repeatedly in 25 percent of these. Menopausal women have an increased risk of recurrent urinary tract infections, which has been associated with low estrogen levels.
Infecting bacteria first come in contact with the inside of the urinary bladder. The bladder lumen is covered with epithelial cells, acting as a fence protecting the vulnerable tissue as well as producing antimicrobial peptides the body’s self-made antibiotic. These peptides act as rapid front line soldiers fighting infecting microorganisms. By the early action of the antimicrobial peptides, the number of bacteria can be reduced before they have a chance to multiply. In the post-menopausal woman, however, the epithelium is fragile and often damaged with occasional gaps between cells, which in turn affect the ability to resist infection.
This research has been funded through grants from the Swedish Research Council, ALF and the Swedish Cancer Foundation, amongst others.
Ovariectomy Decreases Exfoliation Of Superficial Urothelial Cells
One of the first host responses to UPEC infection in the bladder is exfoliation of the superficial urothelial cells containing IBCs into the urine. Although the majority of superficial cells were sloughed into the urine in SHAM mice at 24 h postinfection , a relatively unperturbed superficial layer was evident in OVX mice . Additionally, UPEC staining of the bladders indicated that more IBCs remained in the intact superficial cells in OVX mice than in SHAM mice at this time point. Thus, ovary removal resulted in decreased exfoliation of infected superficial cells at the acute stage , which might contribute to the prolonged UPEC infection.
Don’t Miss: What Are The Signs And Symptoms Of Urinary Tract Infection
Why Utis Increase Post Menopause And What You Can Do About It
More than half of all women develop a urinary tract infection at some point in their life, according to theU.S. Department of Health & Human Services. Unfortunately, once you enter menopause the risk of UTIs increases dramatically.
At Urgent Care of Ada in Ada, Ok, our family medicine specialists have extensive experience in treating UTIs. They offer the following overview and tips for preventing recurrent post-menopausal UTIs.
Rna Isolation Cdna Generation And Quantitative Polymerase Chain Reaction
CFT073 was grown in MSM with or without estradiol statically at 37°C for 6 or 24 h. RNAlater was used before RNA isolation to stabilize the mRNA in CFT073. The E.Z.N.A® Total RNA Kit I was used according to the instructions of the manufacturer for the isolation of total RNA. DNase digestion was conducted according to the instructions of the manufacturer to minimize DNA contamination. RNA concentration and purity were measured with a spectrophotometer before cDNA synthesis. The cDNA synthesis was performed with 100 ng total RNA using the High-Capacity cDNA Reverse Transcription Kit . For the RT-qPCR, 5 ng cDNA and 250 nM of primer were used with Maxima SYBR Green qPCR Master Mix . A CFX96 TouchTM Real-Time PCR Detection System was used for the amplification using the following protocol for 40 cycles: denaturation at 95°C for 15 s, annealing at 60°C for 30 s, and extension at 72°C for 30 s. A dissociation curve between 60 and 95°C was also done after the qPCR. CT values were obtained and the Ct method was used to calculate the fold difference between groups. The results were normalized to the endogenous control glyceraldehyde 3-phosphate dehydrogenase A .
Table 1. Primers used in the real-time qPCR.
Read Also: Menopause Urinary Tract Infection Symptoms
Estrogen Urothelial Stem Cell Niche Activation And Recurrent Utis
UTI recurrence may depend on UPEC’s ability to manipulate differentiation and proliferation of USCs. Thus, the thickened USC layer may provide more protective niches for QIRs to form. These QIRs may hide in the bladder longer due to the slower turnover rate from basal cells to superficial cells. Traditional antibiotic therapies are not effective against bacteria sequestered in QIRs and can also increase the risk of driving the pathogens into quiescence . As these reservoirs are a source of recurrent UTIs, any reduction in their establishment and greater understanding of the interplay between latency and estrogen signaling will have great significance for studying infectious disease in aging female populations.
Estradiol Induces Increased Upec Growth
We began by evaluating the effects estradiol had on the growth of CFT073. We found that 5 pg/ml of estradiol significantly increased the growth of CFT073 compared with unstimulated CFT073 . Statistical significance was reached from 8 h onward for 5 pg/ml estradiol. The biggest growth difference was observed between 5 pg/ml estradiol and unstimulated CFT073 after 24 h . However, the higher concentrations of estradiol did not induce a significant growth increase compared with unstimulated CFT073 .
Figure 1. CFT073 growth with or without the presence of estradiol during 24 h and at 24 h . Data are presented as mean and mean ± SEM of n = 3 independent experiments. The asterisk distinguishes statistical significance: ***p< 0.001 vs. unstimulated CFT073.
Also Check: Best Otc For Urinary Tract Infection
Can Lack Of Estrogen Cause Urinary Incontinence
Incontinence is a common problem, especially among women. But did you know that a lack of estrogen can be to blame? Heres what you need to know about estrogen and incontinence.
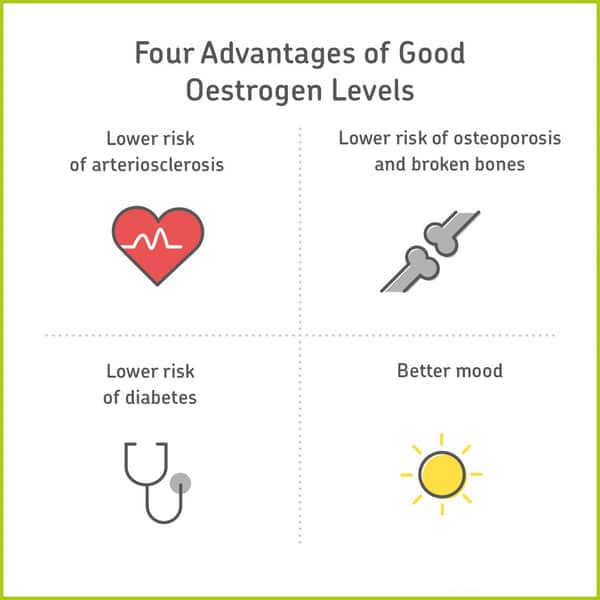
Estrogen is a female hormone that plays an important role throughout the body. It helps maintain bone density, fat distribution, and skin quality. It also relaxes pelvic muscles.
Women who are menopausal experience a significant drop in estrogen, which causes incontinence to become much more common.
Estrogen can also be useful to treat incontinence. Depending on the type of incontinence you have, estrogen may help tighten pelvic muscles or increase bladder control.
Cell And Bacterial Culture
CFT073 is a UPEC strain isolated from a patient with pyelonephritis, which is fully genome sequenced . The bacteria were kept on a tryptic soy agar plate . CFT073 containing an enhanced green fluorescent protein expressing pLMB449 plasmid was used for the colonization experiments.
The bladder epithelial cell line 5,637 is a commercial cell line acquired from the American Type Culture Collection . The cells were grown in Dulbeccos modified Eagles medium with 10% fetal bovine serum , 2 mM L-glutamine, 1 mM non-essential amino acids and incubated at 37°C and 5% CO2 atmosphere. The culture medium was changed during the experiments to DMEM with 2% FBS, 1 mM non-essential amino acids, and 2 mM L-glutamine.
Recommended Reading: Best Tea For Urinary Health
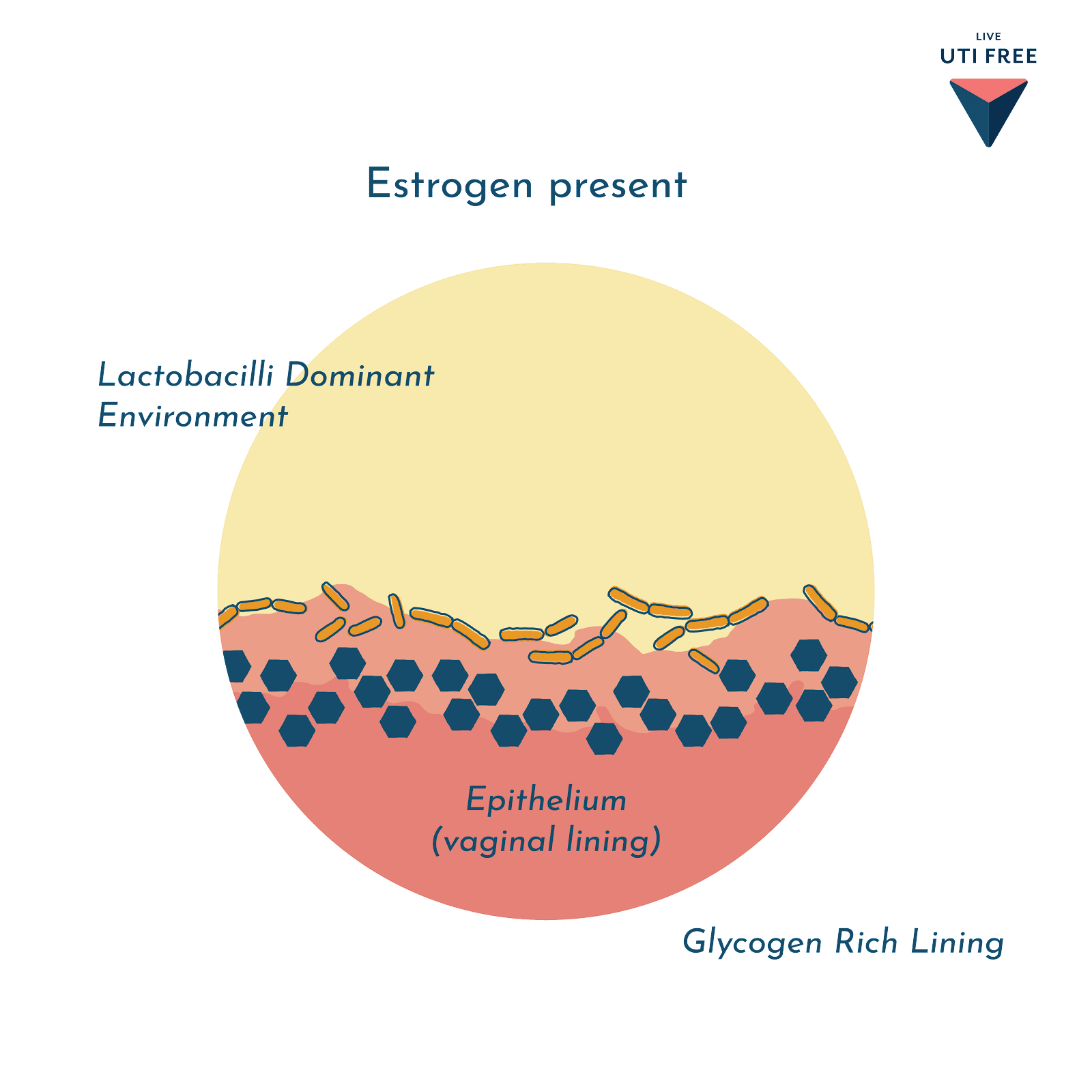
Uti And Menopause May Be Directly Linked To Lactobacillus In The Vaginal Microbiome
What happens after menopause? Studies have shown that post-menopausal females tend to lose Lactobacillusand their vaginal microbiomes become more diverse2-4.
This change can be influenced by Hormone Replacement Therapy .
Studies have shown that post-menopausal females who have been on HRT for years tend to have more of a Lactobacillus dominant community compared to females of the same age not on HRT.
Uti And Menopause: Estrogen May Improve Recurrent Uti
For many people, UTI and menopause go hand-in-hand. But why is post-menopausal UTI a thing? Can estrogen help for recurrent UTI? And is estrogen cream safe?
We get a lot of questions about hormones, hormone therapy and the possible connection to recurrent UTIs.
Many people who reach out to us have noted they experience UTI symptoms at certain times of their menstrual cycle or that the frequency of UTIs increased at the onset of menopause. Others found starting or stopping the contraceptive pill had an impact.
So is there a link between hormones and recurrent UTI, and can we do anything about it?
Jump To Section:
- UTI and menopause: The vaginal and urinary microbiomes. > > > >
- How a healthy vaginal microbiome impacts recurrent UTI. > > > >
- Recurrent UTI and menopause may be linked by estrogen levels. > > > >
- Estrogen vs. antibiotics for UTIs. > > > >
- How estrogen impacts the bladder. > > > >
Recommended Reading: How To Help Cats With Urinary Tract Infections
What Is The Postmenopause
This is the stage of every womans life that follows the menopause, or her last menstrual period.
A woman is definitely postmenopausal when she has not had a period for at least a year. Most women in the UK go through the menopausal transition between the ages of 45 and 55, with the average age of the last menstrual period being about 52.
After the menopause the ovaries cease to produce the main female hormone, oestrogen, and its absence can produce a wide range of symptoms including the below In the long-term lack of oestrogen may predispose many women to:
- Emotional changes
Many women also experience urogenital problems in the years after the menopause. Urogenital problems include the following:
- Urogenital atrophy Vaginal dryness
- Pelvic floor changes and prolapse For more information on prolapse, please visit our main Prolapse Section
- Lower urinary tract symptoms As they get older many women may find they have problems with their urinary tract . Some women may experience OAB leading to problems with urinary urgency. If you would like more information on bladder problems, please visit our main Bladder Problems section
- Recurrent urinary tract infections Commonly called cystitis, this is another form of a waterworks problem. A common symptom of cystitis is a burning pain when passing urine
Also Check: Does Blue Cross Blue Shield Cover Testosterone Therapy
Menopause & Urinary Symptoms At A Glance:
- These urinary changes occur for two reasons: Menopause reduces the amount of the female hormone estrogen, and a lack of estrogen reduces the urinary tracts ability to control urination. Advanced age, which usually coincides with menopause, also has various debilitating effects on the pelvic area organs and tissues.
Recommended Reading: Does Blue Cross Blue Shield Cover Low Testosterone
Don’t Miss: Over The Counter Drugs For Urinary Tract Infection