What Are The Complications After Hysterectomy
Undergoing hysterectomy has consequences for women beyond the obvious surgical risks of performing a hysterectomy, e.g. intraoperative bleeding requiring transfusion, injuring adjacent organs , infection, wound issues, blood clots.
The uterus is the epicenter of what makes you a woman. Women that undergo hysterectomy often struggle psychologically like a man being castrated. There is no way to predict who will suffer like this prior to the surgery.
Risk Factors For The Onset Of Ui Post
In the present study, the number of Cesarean sections and the days of urinary bladder catheterization post-surgery were identified as risk factors for UI post-surgery. Studies of the general female population showed that women with vaginal delivery have a higher frequency of UI than nullipara or those delivering by Cesarean section . It is thought that the increased rate of onset observed in the vaginal delivery group is due to neural damage to the pubococcygeus muscle during delivery and injury to the pudendal nerve . On the other hand, a study of UI in 505 pregnant women followed for 3months after delivery showed that the incidence of UI was significantly lower in the Cesarean section group than in the vaginal delivery group. However, it was reported that there was no significant difference in the rate of UI between those in the vaginal delivery group and women having 3 or more Cesarean sections . The fact that a higher number of Cesarean sections leads to a higher incidence of UI can be explained by the invasion of the abdominal wall during surgery. Repeated surgical invasion of the abdominal wall reduces the activity of the abdominal muscles, which then becomes unable to support the abdominal wall, resulting in lumbar lordosis. The condition in which the abdomen is extended due to the lumber lordosis acts to lower the pressure in the urethra, leading to UI . Therefore, lumbar lordosis may need to be corrected for patients undergoing cesarean section.
How Is Urinary Tract Fistula Treated
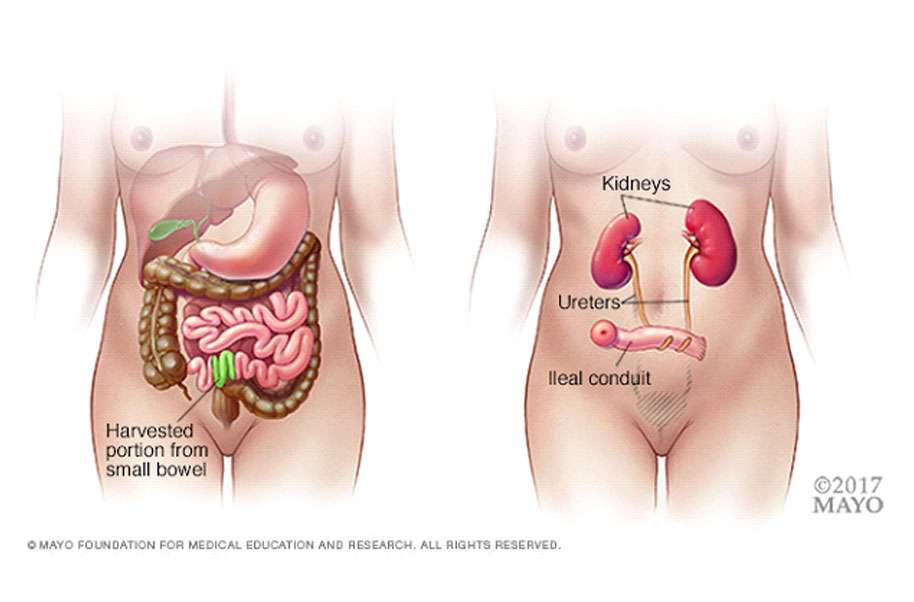
In the past, women would have to wait 6 weeks to 3 months before repairs could be attempted after a traditional open hysterectomy. This is due to the number of adhesions or scar tissue that forms after surgery. This was especially true because the signs of fistula can be delayed for a week to 10 days as the tract forms and this is when the adhesions start to become difficult. A woman would have to wait either with a catheter, a nephrostomy tube , or deal with the leakage until the repair could be attempted.
Robotic-assisted surgery has changed the urologists approach to this life-changing complication. Due to the robotic arms and 10x magnification camera, we are allowed the ability to access the pelvis with great visualization and dexterity. This is done through small incisions as opposed to a large midline incision. Urologists no longer need to wait months to repair the fistula. We can either re-implant the ureter to move it away from the fistula tract in the case of a ureterovaginal fistula or dissect the bladder away from the vaginal wall in the case of a vesicovaginal fistula.
You May Like: Over The Counter Treatment For Urinary Incontinence
How To Prevent Prolapse After Hysterectomy
Resting and Moving About Safely Post-Op
The way you move during your early postoperative recovery affects the load on your pelvic floor after your hysterectomy.
The way you move and engage your muscles during your post-op recovery can affect your pelvic floor after a hysterectomy. It is important that you use techniques that reduce pelvic floor load when you are:
- Rising out of bed or getting into bed
- Moving while in bed
- How you cough or sneeze
- And trying to use the restroom without straining
Avoiding Heavy Lifting
As with any surgical procedure, it is important to not engage in heavy lifting. This can cause additional strain on the pelvic floor. Being cautious when lifting may help reduce the risk of developing prolapse.
Choosing Pelvic Floor Friendly Exercises
Once you have recovered and are at a point when physical therapy and exercise are encouraged, it is important to consider a restorative program that can help you strengthen your core and pelvic region without adding any unnecessary stress and strain.
The Following Factors May Also Contribute To Or Worsen Urinary Incontinence:

- Anatomical factors, including insufficient support of the bladder neck and urethra.
- Neurological factors, such as loss of nerve supply to the pelvic floor muscles or damage to the spinal nerves that control those muscles.
- Behavioral factors, such as smoking and obesity.
- Age is also often cited as an important factor in the development of urinary incontinence.
Recommended Reading: What Are Urinary Tract Symptoms
The Risk For Incontinence After A Hysterectomy
Women who have undergone a hysterectomy have a 60% higher risk of developing urinary incontinence later in life compared to women who havent had one. It often takes years for the symptom to develop after the procedure, because the muscles weaken over time, not right away. Most women who have the operation do so in their 40s and 50s, and they may be over 60 when they begin to experience incontinence.
Hysterectomy May Not Be To Blame
The study is published in the Oct. 27 issue of the journal The Lancet.
“We conclude that hysterectomy, irrespective of surgical technique, increases the risk for stress urinary incontinence surgery later in life,” the researchers write.
But gynecologic surgeon Adam Magos, BSc, MD, is not convinced.
In an editorial accompanying the study, Magos writes that there has been no consensus on whether hysterectomy increases a woman’s risk for urinary incontinence, pointing out that an earlier study from the same research group suggested that it does not.
He notes that the difference in outcomes may be due to the fact that women who have hysterectomies may be more likely to consider surgery an appropriate treatment for stress incontinence.
“Perhaps it has nothing to do with hysterectomy, and women who agree to hysterectomy are just different in ways that we do not yet understand,” he writes.
Show Sources
SOURCES: Altman, D. The Lancet, Oct. 27, 2007 vol 370: pp 1494-1499.Daniel Altman, MD, department of medical epidemiology and biostatistics,Karolinska Institute, Stockholm, Sweden. Adam Magos, BSc, MD, consultantgynecologist, Royal Free Hospital, London.
Read Also: Best Treatment For Urinary Incontinence
What Are The Symptoms Of Urinary Tract Fistula
The main symptom of a urinary tract fistula to the vagina is nonstop leakage of urine. Associated symptoms include abdominal pain or fever if urine collects in the abdomen. The type of leakage associated with a fistula is more severe than the typical stress and urge incontinence that can also occur. In most cases, it requires surgical intervention to repair this complication.
Why Do Hysterectomies Cause Incontinence
Urinary incontinence is a loss of bladder control that commonly leads to urinary leakage, although incontinence may not be experienced until years after the procedure occurs.
Urinary incontinence can happen after a hysterectomy because the procedure affects your pelvic muscles to a great degree. In fact, in an observational study, PubMed reports that 60% of women who undergo hysterectomies have an increased risk of experiencing incontinence.
There are a couple of reasons you may experience incontinence after a hysterectomy.
- Your uterus is near your bladder nerves, and these nerves can sometimes become damaged during the removal of your uterus. Nerve damage is a common cause of incontinence.
- Your uterus keeps the pelvic floor muscles strong and helps support them so they dont sag, which helps support your bladder. When your uterus is removed, the can lead to incontinence.
- Hysterectomies may damage your urinary sphincter, which helps hold your urine in and stops it from leaking. This can lead to incontinence and leakage.
- Your ovaries, which produce the hormone estrogen in your body, may be removed during the surgery. Estrogen helps support your pelvic floor muscles, so when the ovaries are removed and estrogen levels decrease, your pelvic floor weakens, leading to incontinence.
You May Like: Parkinson’s And Urinary Tract Infections
Treatment For Stress Urinary Incontinence
It is important to have your symptoms assessed by a health professional who will assess your bladder behaviour and pelvic floor and confirm that you have stress urinary incontinence.
The main treatment for stress incontinence ispelvic floor exercises. Surgery to tighten or support the bladder outlet can also help. Medication may be used in addition to exercises if you do not want, or are not suitable for surgery.
There is medication available for treating women with moderate to severe stress urinary incontinence, along with pelvic floor muscle exercises. Older people with other problems in addition to their bladder may benefit from seeing a specialist in medicine for older people.
Urinary Retention After Total Laparoscopic Hysterectomy With Immediate Foley Catheter Removal Versus Backfill Void Trial
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : May 5, 2017Results First Posted : October 11, 2018Last Update Posted : October 11, 2018 |
- Study Details
The participant will emerge from anesthesia under routine monitoring and will be transferred to the post-anesthesia care unit when meeting appropriate criteria per anesthesia discretion. A staff PACU nurse will care for the participant in the PACU administer narcotic medications as necessary and/or per participant request. Once the participants are awake and meeting criteria for discharge, the patients in the backfill group will undergo a void trial by a PACU nurse or by a doctor if the nurse is unavailable. About 300 mL of fluid will be instilled into the bladder and the Foley will then be removed. The participant will be given up to 1 hour to urinate and the amount urinated will be recorded using a commode specimen collection measurer. The PVR will be measured using a bladder scanner. If the PVR is greater than 100 mL or if the patient is unable to void within the hour, the void trial will be considered “failed” and a Foley catheter will be replaced.
You May Like: How To Stop Getting Urinary Tract Infections
Treating And Handling Incontinence
There are many options, both surgical and non-surgical, for treating incontinence. There are several types of medication your doctor can prescribe. Your healthcare provider can also explain techniques for bladder retraining, where you develop the ability to hold more urine for a longer period of time. A group of exercises called Kegels, which your healthcare provider can advise you about, can also help strengthen the pelvic muscles. Some women use a device called a pessary, which is inserted into the vagina to support the bladder, and you can use pads to catch leakage that can help eliminate embarrassment and worry. There are various effective surgical procedures that can improve urinary retention.
Visit A Pelvic Floor Physical Therapist
If you are experiencing urinary incontinence, there is a good chance that your pelvic floor muscles may not function properly.
A pelvic floor physical therapist can help you restore function to these muscles, which may help improve your urinary control.
Some benefits of working with a physical therapist include:
- Learning exercises to helpstrengthen your pelvic floor muscles on your own
- Practicing the relaxation of your pelvic floor muscles to maintain bladder control and
- Dealing with stress and anxiety that may contribute to urinary leakage
Rehabilitation of the pelvic floor muscles has been shown to decrease the risk of future urinary tract infections, which is another benefit of visiting a physical therapist.
Read Also: Physical Therapy For Urinary Incontinence
Bladder Or Bowel Damage
In rare cases, there’s damage to abdominal organs such as the bladder or bowel.
This can cause problems such as:
- infection
- incontinence
- needing to pee often
It may be possible to repair any damage during the hysterectomy. You may need a temporary catheter to drain your urine or a colostomy to collect your bowel movements.
What Causes Stress Incontinence After Hysterectomy
Roughly 55,000 hysterectomies are performed in the UK each year. However, the risk of the operation causing urinary incontinence is rarely spoken of.
A hysterectomy actually is the second most common surgery in women, followed by caesarean delivery. The procedure is an operation to remove a womans uterus. This may need to be carried out due to the following reasons:
- Endometriosis
- Cancer of the uterus, ovaries or cervix
- Abnormal vaginal bleeding
Read Also: Can Azo Urinary Tract Defense Get Rid Of Uti
Can A Hysterectomy Affect Your Bladder
Urinaryhysterectomyofthe bladderof thethehysterectomy
Regarding this, can you have bladder problems after a hysterectomy?
A fallen bladder, also known as cystocele or prolapsed bladder, is common after hysterectomies. Prolapsed bladder symptoms include tissue in/protruding from the vagina, problems with urination, increased bladder infections, pelvic discomfort, pain in the lower back, and pain during intercourse.
Furthermore, how long does it take for bladder to heal after hysterectomy? It takes about 6 to 8 weeks to fully recover after having an abdominal hysterectomy. Recovery times are often shorter after a vaginal or laparoscopy hysterectomy. During this time, you should rest as much as possible and not lift anything heavy, such as bags of shopping.
People also ask, can a hysterectomy cause frequent urination?
Bladder and urethral injuries are frequent during operation. After hysterectomy, the most common complication is pelvic floor dysfunction. Urinary incontinence is usually related to bladder or pelvic floor muscles and nerve dysfunction.
What causes bladder pain after hysterectomy?
Up to 81% of patients with CPP will have bladder involvement2 and 79% of women with persistent CPP after hysterectomy are diagnosed with interstitial cystitis. Therefore, interstitial cystitis may be the most common reason for failure of hysterectomy to alleviate pelvic pain.
of aBladdertheAthat the bladder is10 weeksprolapsewhenprolapse can occurearlyhysterectomyfeel
Results Of Individual Studies
Andersen et al., is a 14-year follow-up study describing an objective comparison of SAH and TAH with respect to pelvic organ prolapse and urinary incontinence. It is a randomized controlled trial of patients with benign indications 319 women undergoing SAH or TAH abdominal hysterectomy. Urinary incontinence findings were as follows : objectively assessed urinary incontinence 26.4% and 29.8% subjectively assessed urinary incontinence 39.6% and 34.04% combined subjectively and objectively assessed urinary incontinence 16.98% and 14.89%.
In another study, Andersen et al.,:1767-72.) compared lower urinary tract symptoms following SAH and TAH via exploratory analysis of a 14-year follow-up randomized clinical trial. A total of 197 patients undergoing SAH or TAH hysterectomy for benign uterine diseases answered the questionnaire. Stress incontinence and constant/frequent urinary incontinence were reported in 62.5% and 45%, as well as 33% and 20% of cases .
Another study by Gimbel et al.,:1088-98.) with 1-year follow-up revealed a significantly smaller proportion of women with urinary incontinence 1 year after TAH, as compared to SAH . The lower proportion of women with incontinence in the TAH group reflected the higher proportion of symptom relief as well as a lower proportion of women with new symptoms .
You May Like: What Is The Antibiotic For Urinary Tract Infection
Hysterectomy And Urinary Incontinence: Are They Related
Many women who have had a hysterectomy experience bladder leakage. Typically, women experience post-hysterectomy incontinence months or even years after their procedure.
But are hysterectomy and incontinence related?
The relationship between urinary incontinence and hysterectomy has been studied for decades now.
Findings from two studies show:
- Although it is not usually an immediate issue,women are more likely to experience incontinence later in life, years after having a hysterectomy.
- Hysterectomy surgeryincreases womens risk of developing urinary incontinence in subsequent years.
Women are two times more likely to experience urinary incontinence after a hysterectomy.
Therefore, doctors need to discuss the increased risks of urinary incontinence and possible treatment before having a hysterectomy.
What Can I Do About It
The good news about this is that it is completely manageable and treatable. Here are 7 ways to deal with urinary incontinence after having a hysterectomy.
It isnt unusual for pelvic floor muscles to be weakened after a hysterectomy and its likely that your doctor already introduced you to this treatment method.
Doing Kegels is all about finding the right muscles. One way to find them is by simply pretending to hold your urine or feces. The muscles that were used are the pelvic floor muscles. Then, contract these muscles for about in sets of 10-15 about 3 times daily.
The beauty of this exercise is that there is no need for equipment and it is very discrete. You can incorporate Kegels into your daily life , by performing standing Kegels at your counter or bathroom mirror while you get ready in the morning. You can do them sitting down while youre in bed or make them a part of your workout routine with the bird dog kegel or bridge kegel.
For more advanced Kegels, feel free to add kegel weights. There are many different weights to choose from, of different weights, sizes, shapes, and colors. Finding the right ones to do your Kegels shouldnt be difficult. When choosing Kegel weights, be sure to read the reviews since many are of poorer quality than others and can end up doing more harm than good.
2. Incontinence products
3. Lifestyle changes
4. Injectable implants
5. Medications
6. Sling operations
7. Closing the fistula
Don’t Miss: Are Urinary Tract Infections Painful
The Link Between Hysterectomy And Incontinence
Ahysterectomy is a surgical procedure that removes your uterus. It is an effective treatment for various types of womens health conditions.
But having a hysterectomy could increase your chances of developingincontinence, a condition in which you leak urine.
Here atVirtuosa GYN in San Antonio, Texas, our caring providers would like you to know the relationship between hysterectomies and urinary incontinence. Understanding the connections between the two can help you make the best decisions about your health and well-being.