Implications For Practice And Research
Another challenge in the current clinical practice is the lack of standardised data collection and the absence of a core outcome set for evaluation of surgery for stress urinary incontinence. This affects primary research and limits aggregation of data from primary studies for evidence synthesis. It is incumbent on stakeholders, incontinence related organisations, and researchers to develop core outcome sets and adverse events profile associated with surgery for stress urinary incontinence that are relevant to women, which will aid high quality, multicentre research.
Stress Urinary Incontinence In Women
Stress urinary incontinence is the involuntary loss of urine on effort or physical exertion, including sneezing or coughing1. In women, prevalence ranges from 29 to 75%, depending on age, and two broad pathophysiological mechanisms are proposed: urethral hypermobility and intrinsic sphincter deficiency .
Initial management of SUI includes weight reduction, pelvic floor muscle training and biofeedback4,5. Incontinence pessaries have been used in the past for women who are poor surgical candidates, as has duloxetine, a serotonin and noradrenaline reuptake inhibitor, but neither is recommended by NICE. If conservative management for SUI fails, patients may be offered surgical treatment7. Surgical options for women include urethral bulking agents and bladder neck suspension procedures, including mid-urethral mesh procedures, pubovaginal slings, colposuspension, and the artificial urinary sphincter .
What Are The Types Of Bladder Surgeries
Most bladder surgeries are now done robotically, meaning that your surgeon will just make a small number of incisions and then place ports that allow the use of robotic arms to perform the surgery. Few are open surgeries where theres a long cut. Types of surgeries include:
Bladder cancer is the most common reason for people to undergo bladder surgery. Depending on the stage and progression of bladder cancer, surgery can be used in combination with other therapies such as chemotherapy or radiation therapy. To treat bladder cancer, many different types of procedures may be done. Those procedures include:
Recommended Reading: Treatment After Bladder Tumor Removal
Recommended Reading: Can Being Overweight Cause Urinary Incontinence
Surgery May Benefit Women With Two Types Of Urinary Incontinence
NIH-funded study contrasts with current treatment guidelines.
Surgery for stress urinary incontinence improves symptoms of another form of incontinence, called urgency urinary incontinence, in women who have both types, according to a study supported by the National Institutes of Health. The findings challenge current treatment guidelines, which suggest that the surgery may worsen urgency urinary incontinence in women with both forms, also called mixed urinary incontinence. The study appears in the Journal of the American Medical Association. Funding was provided by NIHs Eunice Kennedy Shriver National Institute of Child Health and Human Development and Office of Research on Womens Health.
Women with mixed urinary incontinence may have more bothersome symptoms than women with either stress or urgency urinary incontinence alone, said Donna Mazloomdoost, M.D., study author and program director of the NICHD Pelvic Floor Disorders Network. The findings show promise in treating a condition that can be hard to manage under existing practices.
Roughly one-third to one-half of all women with urinary incontinence have mixed urinary incontinence. Urgency urinary incontinence results from the spontaneous contraction of bladder muscles, leading to a strong and sudden need to urinate. Stress urinary incontinence occurs when urine leaks out after abdominal pressure increases following a sneeze, cough, laugh or movement, which squeezes the bladder.
NIHTurning Discovery Into Health®
Do Pelvic Floor Muscle Exercises
Strong pelvic floor muscles hold in urine better than weak muscles. You can strengthen your pelvic floor muscles by doing Kegel exercises. These exercises involve tightening and relaxing the muscles that control urine flow. Researchers found that women who received pelvic floor muscle training had fewer leaks per day than women who didnt receive training.6 You should not do pelvic floor exercises while youre urinating.
Men can also benefit from pelvic floor muscle exercises. Strengthening these muscles may help a man leak urine less often, especially dribbling after urination.
A health care professional, such as a physical therapist trained in pelvic floor therapy, can help you get the most out of your Kegel exercises by helping you improve your core muscle strength. Your core includes your torso muscles, especially the lower back, pelvic floor muscles, and abdomen. These muscles keep your pelvis lined up with your spine, which helps with good posture and balance. Your physical therapist can show you how to do some exercises during daily activities, such as riding in a car or sitting at a desk.
You dont need special equipment for Kegel exercises. However, if you are unsure whether you are doing the exercises correctly, you can learn how to perform Kegel exercises properly by using biofeedback, electrical stimulation, or both. Biofeedback uses special sensors to measure muscle contractions that control urination.
You May Like: Stds That Cause Urinary Retention
Surgery For Urge Incontinence
Surgery for urge incontinence due to detrusor overactivity is undertaken only in patients in whom conservative treatment has failed. The aim of surgery is to increase the ability of the bladder to store urine, by increasing its compliance and reducing detrusor contractions. The mainstay of surgical treatment has been augmentation cystoplasty , but the newer modalities sacral neuromodulation and botulinum A toxin have recently been introduced. As a consequence, fewer women now require
Types Of Bladder Surgery
- Bladder Suspension Surgery . A prolapsing, dropping, or sagging bladder is returned to its correct position. It treats stress incontinence, which is urine leakage when a person coughs, sneezes, or laughs. There are several ways to perform bladder suspension surgery. The surgeon may make incisions in the abdomen and pull up the bladder neck. To keep the bladder neck in place, they sew the bladder neck to surrounding tissue or bone. A newer more common method is to use a sling or hammock-like structure to support the bladder neck. The structure can be made out of body tissue or man-made materials such as polypropylene.
- Transurethral Resection with Fulguration. A thin lighted tube called a cystoscope is inserted through the urethra to the bladder. While inside the bladder, surgeons use a tool with a small wire loop to burn away cancer formations. Its effective on tumors as well.
- Segmental Cystectomy. Part of the bladder is removed in segmental cystecomy. It can be performed in some instances of bladder cancer invading the muscle wall. As long as the cancer is only in one part of the bladder, segmental cystectomy is an option.
- Radical Cystectomy. If bladder cancer has spread to the muscle wall or inflicts a large part of the bladder, the patient may undergo radical cystectomy. In this surgical procedure, the surgeon removes the bladder and any lymph nodes or organs that contain cancer.
You May Like: Ways To Help Bladder Infection
Also Check: Azo Urinary Tract Health Gummies
Lifestyle Or Behavioral Changes
If itâs right for your symptoms, your doctor may decide to try changes to your routine and diet first before moving on to medication or surgery.
Bladder training. If you have urgency incontinence , your doctor may tell you to practice holding your urine for a short time when you get the urge instead of going right away. You can start by holding it for 10 minutes. After you successfully do that a few times, you can increase your time. You can also use set times during the day to go, and increase the time in between those regular bathroom trips. You can help your body learn to wait longer by practicing breathing or relaxation techniques. With some effort, you may be able to tame your symptoms and only have to urinate every 3 or 4 hours. Keep in mind that you may not see results right away. But if you stay with it, you should benefit within a few months.
Watching what you eat and drink. Treating your leaks may be as easy as avoiding certain foods and beverages. Cut down on alcohol and caffeine. Many experts believe that these things can irritate the bladder and make urinary incontinence symptoms worse. Cut out coffee, tea, sodas, and alcohol to see if it makes a difference.
Avoiding foods that trigger symptoms. Spicy and acidic foods — like citrus fruits and tomatoes — are common culprits. Others include chocolate and artificial sweeteners. But everyone’s different. You may find food has no effect on you.
Here’s how you do it:
Strength And Limitations In Relation To Other Studies
The current debate on mesh surgery encompasses the treatment of both stress urinary incontinence and pelvic organ prolapse. A statement issued by the US Food and Drug Administration49 and the opinion expressed by the European Commissionâs Scientific Committee on Emerging and Newly Identified Health Risks 50 acknowledge that mesh associated morbidity is higher when treating pelvic organ prolapse, which uses a greater amount of mesh compared with treating stress urinary incontinence. These statements also accept that MUS surgery for stress urinary incontinence is effective and safe in studies with up to one year of follow-up but acknowledge the lack of long term data. Single incision slings have since been removed from the market in Australia51 and New Zealand,52 but this does not affect MUS for the treatment of stress urinary incontinence.
The rate of long term adverse events for MUS has been investigated in recent cohort studies. A large retrospective cohort study in England published in 2017 investigated the rate of complications of vaginal mesh procedures for the treatment of stress urinary incontinence in more than 92â000 women over a period of eight years. The study estimated that 9.8% of women experienced peri-procedural complications, within 30 days or five years, and 5.9% were readmitted at least once for a further mesh procedure within five years of the index procedure.16
Read Also: Can An Iud Cause Urinary Tract Infections
Viii Key Informants/technical Experts And Review Of Key Questions
Key Informants are the end users of research and include patients and caregivers, practicing clinicians, relevant professional and consumer organizations, purchasers of health care, and others with experience in making health care decisions.
Technical Experts constitute a multidisciplinary group of clinical, content, and methodological experts who provide input in defining populations, interventions, comparisons, and outcomes and identify particular studies or databases to search. They are selected to provide broad expertise and perspectives specific to the topic under development.
Key Informants and Technical Experts were included in a multi-stakeholder virtual workshop by PCORI in December 2016. The workshop reviewed scoping for the updated review, prioritization of key questions, and a discussion of where the evidence base has accumulated since the prior review and emerging issues in UI. This UI protocol was developed based upon the findings of the multi-stakeholder virtual workshop. Key Informants and Technical Experts do not do analysis of any kind nor do they contribute to the writing of the report. They have not reviewed the report, except as given the opportunity to do so through the peer- or public-review mechanism.
Monalisa Touch For Urinary Incontinence
MonaLisa Touch is a painless vaginal laser treatment that delivers CO2 laser energy to the vaginal walls using a slender wand. It is an effective, state-of-the-art treatment for stress urinary incontinence as well as vaginal dryness, itching & irritation, and painful sex.
Flint ObGyn was one of the first gynecology offices in Genesee County to make this ground-breaking and life changing nonsurgical treatment available to our patients.
The estrogen in a womans body helps keep her vaginal tissue supple and moist. As hormone production decreases with age, menopause or as a result of surgery or medications, vaginal atrophy begins to occur.
Stress incontinence occurs when the pelvic tissues and muscles that support the urethra at the opening of the bladder become weaker due to pregnancy, weight gain, hormonal changes, injury or aging.
The rejuvenated vaginal tissue also generates more lubrication, reducing painful dryness and remedying painful sex. And, the improvement in vaginal tightness also improves sexual sensation for both the female patient and her sexual partner.
MonaLisa touch treatments for urinary incontinence are non surgical, and non-hormonal. There are no known side effects, and absolutely no downtime.
You May Like: What Is Best Antibiotic For Urinary Tract Infection
Eligibility Criteria For The Key Questions
The eligibility criteria for the update are not substantially different from the criteria for the 2012 AHRQ review. The main differences relate to dropping KQ 1 , explicitly adding subpopulations of interest, and making some criteria more explicit .
Changes from the 2012 AHRQ review include the following:
Population
Based on stakeholder input, we will highlight four specific subpopulations of interest . Studies that either focus on these subpopulations or provide relevant subgroup data will be highlighted.
In addition, we will apply stricter rules about the exclusion criteria, allowing only up to 10 percent of study participants to be among the excluded populations the 2012 AHRQ review allowed up to 25 percent to be men. If we find studies that were included in the 2012 AHRQ review that included between 10 and 25 percent men, we will exclude these from the current review.
Interventions
Comparators
No changes are made from the 2012 AHRQ review.
Outcomes
All outcomes reported in the 2012 AHRQ review’s eligibility criteria are included in this update, except for urodynamic testing, which is used in practice only for diagnosis, not for followup outcome assessment. We will add patient-centered outcomes identified from the contextual question on how patients define outcome success.
Study design, Timing, Setting
No substantive changes are made from the 2012 AHRQ review.
| Unable to read or translate. |
Data Extraction And Assessment Of Risk Of Bias
Cochrane reviews provided outcome data from individual randomised controlled trials, study characteristics, and findings of risk of bias assessment. We cross checked the primary outcome data against primary trial reports, whereas all other data, including adverse events, were extracted verbatim from the Cochrane reviews. One reviewer extracted data from new studies identified by the literature searches, and another reviewer independently verified these against primary trial reports for accuracy and completeness, with risk of bias assessed using the Cochrane risk of bias tool.39 Authors of Cochrane reviews attempted to contact investigators of primary studies to obtain key missing data this was not required for the new studies identified by the updated literature searches.
Read Also: Does Cvs Minute Clinic Do Urinary Tract Infections
Conservative Treatments For Urinary Incontinence
When it comes to non-surgical treatments for urinary incontinence, the options depend largely which type of incontinence is present. Generally, the primary treatment is pelvic floor muscle training . However, if the symptom is stress incontinence, the focus is placed on strengthening the pelvic floor due to hypotonicity. In the case of overactive bladder, the focus is placed on pelvic floor relaxation combined with other treatments such as bladder retraining. On this page, we will review all of the treatments offered for the different types of urinary incontinence. You should always speak to your doctor or pelvic floor physical therapist if you have incontinence and they will guide you to the right treatments for you.
Regardless of whether your doctor suggests conservative treatments or more invasive surgical options, PFMT is always required. To have surgery without undertaking rehabilitation of your pelvic floor muscles is the equivalent to treating the symptom without addressing the root cause. Training your muscles will help to rebalance the pelvic floor to overcome hypertonicity or hypotonicity bringing the pelvic floor back to a normal resting state.
Stress & Urinary Incontinence Treatment Options
Several stress incontinence treatment exists and our team of doctors and womens health physiotherapists will recommend treatment for incontinence based on several health factors including age, condition and severity of urinary symptoms.
Sometimes it might be necessary to conduct a bladder operation however these procedures are commonly carried out with manageable symptoms and normally have a quick recovery time with the right after care. Read more about incontinence treatments below.
Read Also: How Do You Treat A Urinary Tract Infection At Home
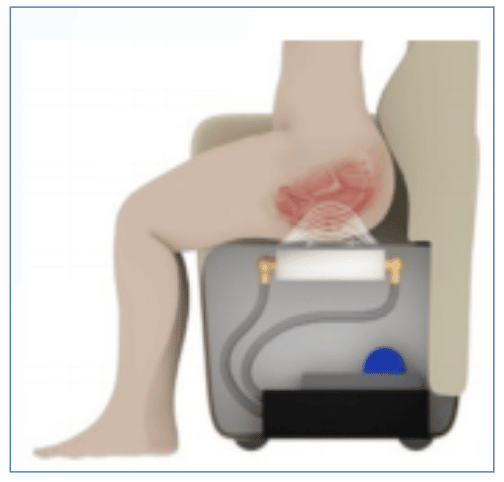
Percutaneous Tibial Nerve Stimulation
Percutaneous tibial nerve stimulation involves stimulating the sacral nerve plexus for 30 minutes weekly for 12 weeks by placing a needle percutaneously into the posterior tibial nerve peripherally16. A 2018 systematic review of PTNS found rates of success of between 54 and 79%, depending on the definition of success12. An RCT comparing PTNS with tolterodine found that 79.5% of patients with PTNS had a subjective cure or improvement in symptoms at 12 weeks compared with 54.8% of the tolterodine group, suggesting that PTNS may be a reasonable alternative to anticholinergics17. MacDiarmidet al. followed up the patients who had responded to PTNS, further treatment being given on demand, and found that the effects of PTNS were sustained between 3 and 12 months18. Despite encouraging data, long-term data for PTNS are sparse most studies provide data to 12 weeks only and use varying definitions of success.
Types Of Bladder Surgery For Incontinence
Sometimes incontinence can have an adverse effect on your quality of life.
When youve exhausted conventional treatments and the ever-present symptoms still pose as a major disruption to your every day activities, it may be time to look at a more radical solution, like surgery.
Although it is more invasive and has a higher risk of complications than other therapies, urinary incontinence surgery can also provide a long-term solution in severe or persistent cases.
Your surgical options depend on the type of urinary incontinenceyou have. Most options for urinary incontinence surgery treat stress incontinence. However, surgical alternatives are available for other bladder problems, including urge incontinence.
Read Also: Green Tea For Urinary Tract Infection
How Is Urinary Incontinence Managed
Your GP will first suggest making lifestyle changes to improve symptoms, including weight loss and cutting down on alcohol and caffeine. Pelvic floor exercises are also recommended to strengthen pelvic floor muscles, which often weaken following childbirth or as a natural result of ageing.
Many women also benefit from using incontinence products, like pads, absorbent pants, or handheld urinals. Sometimes, medicine may be prescribed to help manage symptoms.
If these measures fail, you may be referred for bladder training, guided by a specialist who can help teach you ways to train yourself to wait longer to pass urine.
In some cases, medication or surgery may be the best option where all other means have been unsuccessful.