How Is Neurogenic Bladder Diagnosed
If your healthcare provider thinks you may have neurogenic bladder, he or she will want to check youre your brain, spinal cord, and bladder. He or she will review your health history and do a physical exam. Other tests may include:
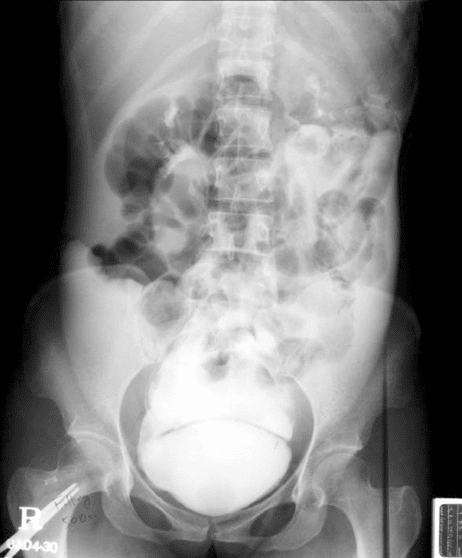
- X-rays of the skull and spine. This imaging test uses invisible energy beams to make images of tissues, bones, and organs.
- Imaging tests of the bladder and ureters
- Ultrasound . This imaging test uses high-frequency sound waves to create images of the organs on a computer screen.
- Cystoscopy. Your healthcare provider puts a thin, flexible tube and viewing device in through the urethra to examine the urinary tract. It checks for structure changes or blockages, such as tumors or stones.
- Tests that involve filling the bladder, such as urodynamics. These tests show how much the bladder can hold and check to see if it fully empties.
Read Also: E Coli In Urinary Tract
What Is Bladder Management
Bladder management is an ongoing set of treatments and practices that help keep your bladder and kidneys healthy and free from infection and other problems.
- Bladder management cannot fix or solve the problems caused by your SCI, but it can help you manage them to improve your health and quality of life. With appropriate management you can prevent incontinence and damage to the kidneys.
- You can work with your doctor to choose which bladder management option fits into your lifestyle and maintains bladder and kidney health.
What Are The Potential Complications Of Difficulty Urinating After Surgery
The main complication of postoperative urinary retention is overfilling the bladder, which can stretch the bladder muscles too much. This injures the bladder muscles. In most cases, the damage is temporary, but it can be permanent. There are also potential complications of catheterization, including bladder infection.
Recovering from POUR can take time. Most people will regain the ability to urinate within 1 to 3 days. It usually resolves once the effects of surgery and other contributors wear off.
Also Check: How Long To Get Rid Of Urinary Tract Infection
Healthy Bladder Function After Anesthesia
Structure of the Urinary Bladder .
A healthy bladder is a fairly complex, sac-like organ. Composed of a body and a neck, the bladder is made of different types of muscle fibers and nerves that interact to allow micturition, or the passage of urine. Emptying the bladder requires input and action from the bladder, surrounding muscles, spinal cord, brainstem, and brain.
The bladders body holds the urine. There are stretch receptors in the walls of the bladder body that indicate the level of fullness of the bladder. These special sensors send signals to the brain when the bladder should be emptied. The neck of the bladder has sphincters or valves that open to allow urine to be expelled.
- The internal urethral sphincter, located inside the neck of the bladder, is made of smooth muscle fibers and is not under voluntary control.
- The external urethral sphincter is a ring formed by the pelvic floor muscles and is under voluntary control.
Spinal Anesthetics For Cesarean Section

Spinal anesthetics are used very often for Cesarean sections. The side effect I hear about most in these cases is shortness of breath.
During Cesarean delivery, the mom is laid flat on the bed, tilted to the left side a bit. The arms are extended out perpendicular to the body. Often the neck feels “crowded” by large breasts and a fully pregnant belly in this position. In other words, everything is pushed upwards.
It would be difficult under the best of circumstances for a full-term pregnant woman to feel like she can breathe well in this position. With the addition of a numb chest wall, it’s easy to see why this feeling is so common and often can induce panic if the woman isn’t reassured that the monitors show she is actually breathing well. If they still aren’t convinced, I show them the fog in the oxygen mask as they breathe. This usually works well until the OB begins to push on the upper abdomen to deliver the baby. Luckily, this actual obstruction to deep breathing ends quickly, and when mom hears the beautiful sound of her baby crying for the first time, she forgets all those unpleasant sensations!
Recommended Reading: How Long Does Urinary Incontinence Last
Working On A Manuscript
Neuraxial anesthesia can result in significant bladder denervation in the perioperative period and can subsequently precipitate urinary retention.1 The dysfunction associated with this transient effect ranges from mild to severe . When alleviated with catheterization, urinary retention can increase morbidity by introducing infection and increasing the length of hospital stay.2–5
Urinary retention is the inability to initiate micturition or to empty the bladder completely. There are no clear defining characteristics of urinary retention, such as a specific volume of urine or elapsed time postoperatively without micturition however, in accordance with the consensus view in the contemporary literature, urinary retention would be described as an inability to initiate micturition with a bladder volume exceeding 500 mL.6 Urinary retention can be complete or partial, acute or chronic, painful or silent, obstructive or non-obstructive. Overflow incontinence secondary to excess intravesical pressure can occur. De novo incontinence secondary to sphincter damage, detrusor overactivity , or stress developing in the perioperative period are uncommon occurrences. The long-term consequences of postoperative urinary retention are not always immediately apparent in the perioperative period, although increased hospital length of stay and prolonged detrusor dysfunction have been documented.1,6
Mechanical Techniques To Manage Bladder Emptying
There are three proposed methods employed to empty the bladder in dogs following spinal cord injury: manual emptying intermittent aseptic catheterization and placement of a indwelling catheter.
Intermittent sterile catheterization is also simple, guarantees an almost complete bladder emptying. But it is more invasive, carries a risk of introducing an infection in the bladder, can potentially cause urethral inflammation and stricture if done frequently, and might also appear challenging to untrained staff in particular in female dogs. In female dogs, the clinicians’ preference might also often be to leave indwelling catheter in place rather than repeating sterile catheterization.
Placement of an indwelling catheter has similar advantages and disadvantages with the previous method but can lead to bladder mucosa minor trauma and bleeding , therefore blocking the catheter. It is usually used for a short time during hospitalization because it will be difficult for the owner to manage it at home. The use of a closed bag system and long-term placement of the catheter removes the need for repeated catheterization and is comfortable for the nursing team and the dog, also reducing the risk of urine scald especially for large dogs.
Recommended Reading: Urinary Tract Infection Women Antibiotics
How Long Does Incontinence Last
One thing you should know is that most men regain continence following prostate surgery. If youre between the ages of 40 and 60, and generally healthy, the outlook is particularly good. In such cases, most men are no longer experiencing incontinence after about three months.
For others, it takes closer to a year. In such cases, there are effective treatments.
You May Like: Can Urinary Tract Infection Go Away Without Antibiotics
Bladder Management Options Following Sci
What you need to know?
- Your spinal cord injury might limit your ability to control your urine. You might not be able to stop urine from flowing, or you might not be able to release it.
- Uncontrolled urination or inability to empty your bladder can have a negative effect on your quality of life and cause bladder and kidney infections and other problems.
- Appropriate bladder management can help keep your bladder and kidneys healthy.
- Each type of bladder management option has pros and cons.
- Your doctor can help you choose the bladder management option that best meets your needs and lifestyle, and keeps your bladder and kidneys healthy.
Recommended Reading: What Causes Urinary Dribbling In Males
How Is The Cause Of Difficulty Urinating After Surgery Diagnosed
Since symptoms of urinary retention are not always present, the postoperative care team will monitor your ability to urinate. You may have a urine collection pan in the toilet you use to measure how much you are voiding. In general, you should not go for longer than 6 to 7 hours without urinating. If you are unable to urinate, a physical exam may reveal a distended bladder. Sometimes, the care team may use ultrasound to view the bladder. Using a catheter to drain the bladder and measure its contents is useful for both diagnosing and treating POUR.
A Herniated Disc Can Cause Incontinence: Heres What You Need To Know
A herniated disc is a medical condition that occurs when the gel-like center of a spinal disc ruptures through a tear in the discs outer layer. This can cause severe pain and other symptoms. In some cases, a herniated disc can also cause incontinence. There are a few different ways that a herniated disc can cause incontinence. One is by pressing on the nerves that control the bladder. This can cause the bladder to spasm and leak urine. Another way is by causing an inflammation of the bladder. This can also lead to incontinence. Incontinence can be a very embarrassing and inconvenient symptom of a herniated disc. If you are experiencing incontinence, it is important to see a doctor so that they can determine the best course of treatment. Treatment options may include pain medication, physical therapy, and surgery.
Lower extremity symptoms and signs associated with low back pain are uncommon, but bladder and bowel problems are rarely seen. The patient presented here is a 61-year-old woman who only had fecal incontinence as a result of a large LDH. In less than a day, a significant amount of her deficit was corrected through urgent decompression and diskectomy. Approximately 0.12% of the LDHs are expected to test positive for CES. Cerebroventricular radiculopathy is caused by bladder and/or bowel dysfunction, saddle anesthesia, sexual dysfunction, and L5-S1 radiculopathy. Symptomatic relief is provided by an urgent/emergent diskectomy in patients like this one.
Recommended Reading: Get Rid Of Urinary Tract Infection Naturally
How Can I Know If My Bladder And Sphincter Are Working Correctly
Doctors can do a urodynamics test to see how well your bladder and sphincter are working:
- A catheter goes up through your urethra into the bladder.
- Your bladder is slowly filled with fluid.
- Doctors then measure how your bladder and sphincter respond to the fluid in the bladder.
- The test can help inform which bladder management option is best for you.
Related Factsheets
Respiratory Effects Of Spinal Anesthesia
In patients with normal lung physiology, spinal anesthesia has little effect on pulmonary function. Lung volumes, resting minute ventilation, dead space, arterial blood gas tensions, and shunt fraction show minimal change after spinal anesthesia. The main respiratory effect of spinal anesthesia occurs during high spinal block when active exhalation is affected due to paralysis of abdominal and intercostal muscles. During high spinal block, expiratory reserve volume, peak expiratory flow, and maximum minute ventilation are reduced. Patients with obstructive pulmonary disease who rely on accessory muscle use for adequate ventilation should be monitored carefully after spinal block. Patients with normal pulmonary function and a high spinal nerve block may complain of dyspnea, but if they are able to speak clearly in a normal voice, ventilation is usually adequate. The dyspnea is usually due to the inability to feel the chest wall move during respiration, and simple assurance is usually effective in allaying the patients distress.
Read Also: Azithromycin Urinary Tract Infection Dose
Possible Mechanisms Underlying Recovery
Reorganization of the micturition reflex following spinal cord injury is dependent in part on the plasticity of bladder afferent pathways and the unmasking of reflexes triggered by unmyelinated, capsaicin-sensitive, C-fiber bladder afferent neurons. Plasticity of bladder afferent neurons is associated with morphologic, chemical, and electrical changes, which appears to be mediated in part by neurotrophic factors released at the level of spinal cord and the peripheral target organs . Upregulation of anti-inflammatory mediators and neuroprotective molecules is likely to play an important role in the plasticity of bladder afferent pathways as well as reorganization of synaptic connections in the spinal cord . In rats, poor voiding efficiency at 4 and 8 weeks after spinal cord injury was coincident with upregulation of pro-inflammatory cytokines , chemokines and downregulation of anti-inflammatory cytokines IL-4 and IL-13, whereas spontaneous recovery of voiding function at 12 weeks was associated with maximum expression of anti-inflammatory cytokine IL-1018, neurotrophin BDNF and CXCL-5 as well as the neuroprotective leptin19 in bladder .
How Is Cauda Equina Syndrome Diagnosed
Your healthcare provider will diagnose your cauda equina syndrome by interviewing you about your symptoms, assessing your physical abilities, performing tests and ordering imaging tests. Theyll assess your abilities by having you:
- Displaced spinal cord or nerves because of herniated disks, bone spurs and tumors.
Youll be diagnosed with cauda equina syndrome if you have two sets of symptoms:
- Bowel, bladder and/or sexual problems.
- Paresthesia of the backs of your legs, butt, hip and inner thighs.
Recommended Reading: Urinary Tract Infection Men Remedies
What Questions Should I Ask My Healthcare Provider About Cauda Equina Syndrome
- What type of cauda equina syndrome do I have?
- What classification of cauda equina syndrome do I have?
- How quickly do I need surgery?
- How long will the surgery take?
- How long will I be in the hospital after surgery?
- Do I have a herniated disk?
A note from Cleveland Clinic
Cauda equina syndrome affects about 1 out of 65,000 people. Its uncommon, but its important to pay attention to the red flag symptoms because they might indicate various health issues. Be on the lookout for numbness in your saddle area, pain in your back and legs, problems with peeing or pooping, difficulties with sex and weakness in your extremities. See a healthcare provider immediately if you have these symptoms.
Learning that something is compressing the nerves in your back would frighten anyone. But donât hesitate to go to the emergency department if you experience symptoms. The faster you get treatment, the less likely youll have permanent damage to your body, including incontinence and paralysis.
Last reviewed by a Cleveland Clinic medical professional on 11/22/2021.
References
Also Check: Amoxicillin 500mg For Urinary Tract Infection
Consequences Of Spinal Cord Injury On Gastrointestinal Function
Fecal incontinence is a more common problem in dogs that suffer acute contusive or vascular lesions of the spinal cord, such as acute nucleus pulposus extrusion or fibro-cartilaginous embolism, respectively compared to compressive lesions. This might be because parenchymal lesions are more centrally located within the spinal cord or perhaps resulting from dilation of the spinal canal. This is seen in dogs with chronic compression of the spinal cord from sub-arachnoid diverticulum, such as in Pugs where fecal incontinence is common. The prognosis for dogs with acute contusive or vascular lesions is further discussed in the treatment section below.
You May Like: Can Drinking Lots Of Water Cure A Urinary Tract Infection
What We Found And What This Means
We found factors associated with PO-UR included being older, male, and having previous urinary problems or long-term enlargement of the prostate gland restricting the ability to urinate . Reducing fluids and using a catheter during surgery were associated with a lower risk of PO-UR.
Giving tamsulosin before surgery can reduce the number of people who develop PO-UR. All the studies of tamsulosin were in men and none were in UK settings, so more studies are needed to see if similar effects are found in women and in UK settings.
Replacing or avoiding morphine in the anaesthetic, administering the anaesthetic in certain ways, and getting patients up and moving as soon as possible after their operation reduced the chance of developing PO-UR. For people who developed it, a small number of studies also suggested that a hot pack or warm gauze and a warm coffee could help.
Based on the results of our review, we developed an intervention to reduce the risk of developing PO-UR the PO-UR prevention package. This package involves providing hospital staff with training and advice to:
- Avoid using morphine or reducing the dose, wherever possible
- Change other aspects of the anaesthesia or analgesia
- Get people moving as soon as possible after their operation
- Reduce fluids as far as is safe, before and during the operation
- Provide a hot caffeinated drink and hot pack placed on the abdomen around two hours after the operation
What Does My Spinal Cord Have To Do With My Bladder
- Your brain sends and receives signals through your spinal cord. At the lowest part of your spinal cord is an area called the sacral micturition center that has nerves attached to it that go to and from the bladder. These nerves help to signal the brain when the bladder needs to be emptied. They also control the sphincter.
- For example, if you need to hold your urine until a convenient time to empty your bladder, your brain will signal the bladder not to squeeze and the sphincter to tighten so that you can wait. When it is time to release your urine, signals from your brain will then send signals down your spinal cord to squeeze the bladder and relax the sphincter. If an SCI has damaged the spinal cord, the signals from the brain to the bladder do not work correctly and you might not be able to control your urine. You might not be able to stop urine from flowing , or you might not be able to release it .
Also Check: Royal Canin Feline Urinary Calm