How To Know If You Are Suffering From Vaginal Mesh Complications
Pelvic organ prolapse is an often-frustrating condition that many women experience after childbirth and with changes linked to menopause, obesity, persistent cough or constipation that strains your muscles, and other common issues.
Its caused by weakening of the pelvic floor muscles that normally hold your uterus, urinary bladder, and other pelvic organs in place. As these muscles stretch and weaken, your pelvic organs can begin to droop out of place. Though not typically life-threatening, pelvic organ prolapse can cause severe urinary incontinence , painful sexual intercourse, fecal incontinence , and other life-altering issues.
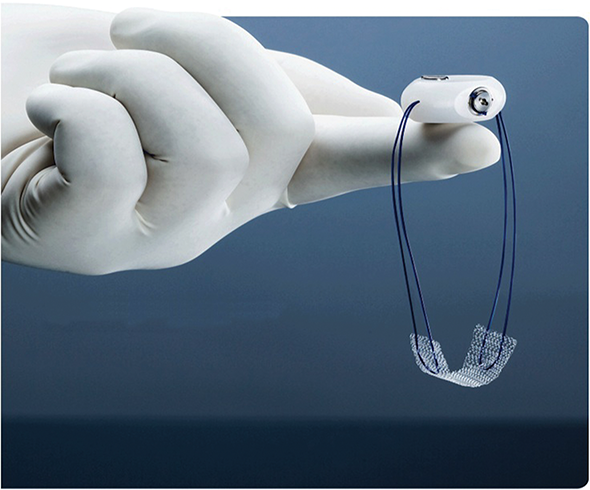
Depending on the extent of the prolapse, doctors may recommend transvaginal mesh surgery to help resolve your symptoms. The mesh is a surgical material that is implanted during the procedure and designed to reinforce the vaginal walls and supply support for your bladder and urethra. Transvaginal refers to the surgical approach and may be suggested because its minimally invasive and eliminates the need for external incisions.
Read on to learn what he has to say about the complications and symptoms you may experience after vaginal mesh surgery.
Read Also: Bcg Chemo For Bladder Cancer
What Happens After The Male Sling Procedure
Following your surgery, you may have a catheter exiting from the urethra for a short period of time. The catheter is in place to allow you to empty your bladder since there may be swelling after surgery that makes it difficult to urinate. After the swelling goes down, you will gradually be able to urinate on your own and empty your bladder well. However, your normal pattern of urination may not return for a few weeks. You can resume a normal diet after surgery.
How Is The Male Sling Procedure Done
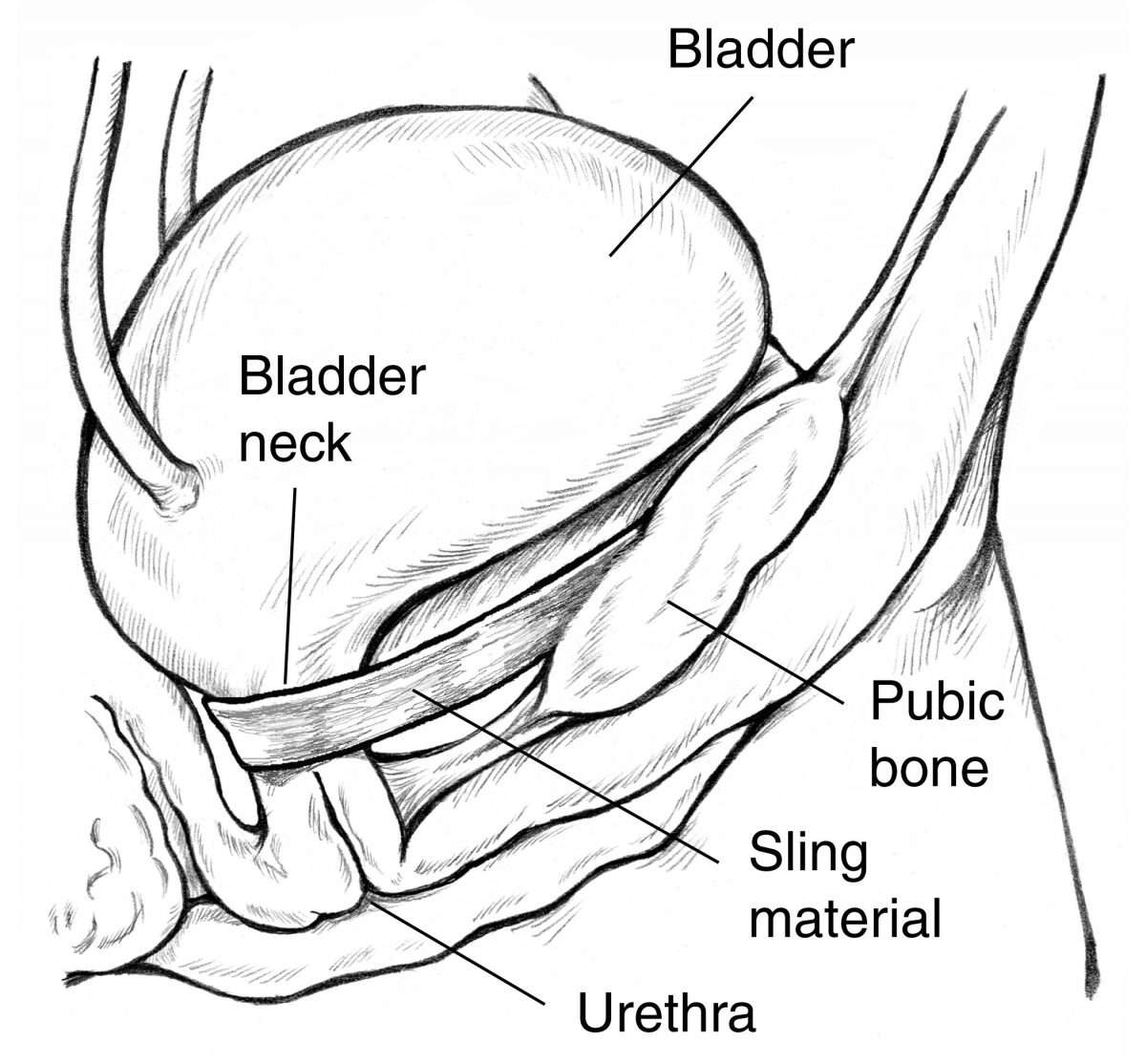
During the male sling procedure, an incision is made through the perineal tissue . The surgeon will then expose the urethra and use a supportive sling around part of the urethral bulb that covers the most upper part of the urethra close to where it enters the area of the urethral sphincter. By wrapping the surgical tape around the urethral bulb, the sling gently moves the urethra into a new position and increases resistance in this area. This lends support to the bladder neck. This procedure has been shown to help with mild to moderate urinary incontinence, and is most commonly used after radical prostatectomy.
The male sling procedure is usually performed as an outpatient surgery. However, there are some cases where patients will need to stay in the hospital overnight after surgery. The sling support requires absorbable sutures in the perineum . This may cause some pain right after surgery, but overall, the amount of pain is usually mild and well tolerated.
You May Like: Cll And Urinary Tract Infections
The Importance Of Patient Factors
We also reserve slings for men that have a Valsalva leak point pressure greater than 60cmH2O. Our group has previously demonstrated that VLPP greater than 70cmH2O is an indicator of success, but anecdotally we have found that patients with greater than 60cm water pressure also do well . Furthermore, Barnard et al. found that a VLPP greater than 100cmH2O, compared to less than 100cmH2O, was associated with a higher degree of success .
Finally, we do not offer a sling to men who have a history of pelvic radiation. While success has been reported to be 51-73% with the AdVance® sling, Bauer et al. found a cure rate of just 25% and a failure rate of 50% in irradiated patients . Our group thinks that there are enough studies to suggest poor sling outcomes in men with a history of radiation. While most studies have been underpowered, both Rehder et al. and Cornu et al. found a higher failure rate in irradiated patients compared to non-radiated .
Is Pelvic Mesh Safe What Patients Need To Know
Synthetic material used to help treat a common condition has been linked to problems and lawsuits. A Michigan Medicine board-certified urogynecologist explains the issues.
Questions surrounding pelvic mesh could leave some women feeling trapped.
Mesh material, used to treat pelvic organ prolapse and stress urinary incontinence, was marketed by its manufacturers as a durable surgical method for repairing these challenging problems compared to other corrective surgeries with a high failure rate.
ASK ALEXA: Add the Michigan Medicine News Break to Your Flash Briefing
But pelvic mesh has faced increased scrutiny from the U.S. Food and Drug Administration due to reports of frequent postoperative complications. Thousands of patient lawsuits have been filed citing mesh-related pain, bleeding and infection, among other problems.
Women should be informed but not necessarily fearful, says Megan Schimpf, M.D., an associate professor of obstetrics and gynecology and urology at the University of Michigan.
We dont want to get the message out there that all mesh is bad, or that mesh has to be removed simply because other women are having problems, Schimpf says, noting that some problems with mesh surgery may be related to how it was placed or surgeons lacking training or experience.
Many women are happy and symptom-free after mesh surgery.
Prolapse surgeries where mesh is implanted through the vaginal opening have the highest risk of complications.
Recommended Reading: Urinary Tract Infection And Alcohol
Questions About Pelvic Mesh
Is pelvic mesh safe?
Schimpf: I do think that its safe when used in the right hands in the right patients.
Mesh is made out of a suture material that has been used widely in surgery and medicine for many years. That material is woven into a fabric that has been used in many procedures, including cardiothoracic surgery and hernia surgery.
Mesh surgery for stress urinary incontinence is often thought of as the gold standard or best surgical option for this problem. Risks are low, and my patients are so happy after this procedure. Many are out running marathons, playing with their grandkids and living their life again without leakage after that surgery.
Prolapse mesh is safe, too. Here at Michigan, we only place mesh through the abdominal wall, using our laparoscopic skills to do this without any major incisions. My patients after this surgery are also extremely happy. Some of them dont even feel like theyve had surgery. We dont perform the vaginal mesh surgery that has caused more complications.
So, I dont think theres any inherent risk in having mesh placed, but there are specifics that a woman needs to know about what surgery shes having. As long as you truly have a problem and have a surgeon well-versed in using it mesh can help.
What women should consider surgery for prolapse or incontinence? Is it the only option?
SEE ALSO: A Female Urologist Explains Womens Most Common Urological Concerns and How to Treat Them
What can go wrong?
Complication Rates By Type Of Sling
Before undergoing bladder sling surgery, women should ask their doctors about the technique they plan to use. Complication rates may vary depending on the type of mesh sling and technique.
A 2010 study of bladder sling procedures by Z. Chen and colleagues published in Urologia analyzed the outcomes of 187 women who received bladder slings to treat stress urinary incontinence. Authors found that transobturator vaginal tape inside-out and transobturator vaginal tape out-inside are simpler techniques with fewer complications compared to tension-free vaginal tape .
Women who used TVT had an average hospital stay of five days versus about two days for the TOT group.
The complication rate in the study was:
- 15.6 percent for tension-free vaginal tape
- 9.20 percent for transobturator vaginal tape inside-out
- 8.90 percent for transobturator vaginal tape out-inside
Complications from the procedures included discomfort with urinating, bleeding outside blood vessels and dysfunction of lower limbs. TVT was the only procedure associated with bladder perforation. Despite the complication rate, doctors found the slings safe.
The three tension-free urethral suspension techniques have similar efficacy, all of them are safe and effective procedures for the treatment of female SUI, authors wrote.
Recommended Reading: Hills Feline C D Urinary Stress
General Principles Of Management Of Mesh And Graft Complications
Approaches to management of mesh-related complications in pelvic floor surgery include observation, physical therapy, medications, and surgery. Table 1 presents an overview of specific mesh and graft complications and management options. There may be settings in which observation of exposed mesh is reasonable 4. Surgical intervention or referral is not always necessary for type 1 mesh exposures into the vagina. Asymptomatic exposures of monofilament macroporous meshes can be managed expectantly. For women with symptoms, a trial of vaginal estrogen can be attempted for small mesh exposures. Topical estrogen may improve or resolve the mesh exposure, though there is little prospective, comparative evidence supporting this approach. A period of 612 weeks is a reasonable period to try topical estrogen.
One multicenter study of mesh complications after reconstructive surgery found that 60% of women required two or more interventions and that the first intervention was surgical in approximately one half of cases 5. These procedures are complex and should be approached with caution. Surgeons who are unfamiliar with the original index procedure or the management issues that follow should refer the patient to a surgeon who is familiar with these types of repairs.
Try Lifestyle Changes First
Sometimes women can change their habits to decrease the incontinence to the point that it isnt bothersome. If you smoke, drink multiple cups of coffee, or are overweight, you can often lessen incontinence by not using tobacco, limiting your coffee intake, and losing weight. If youve tried these lifestyle changes and arent getting results, there are other options, including urinary slings.
Recommended Reading: Can You Get Urinary Tract Infection From Sex
What Will Happen During Surgery
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given local anesthesia to numb the surgery area. With local anesthesia, you may still feel pressure or pushing during surgery, but you should not feel pain.
- Your surgeon will make an incision in your perineum. This is the area between your scrotum and anus. He or she will place the sling under your urethra. The sling may have 2 ends or 4 ends. The ends may be stitched to your abdominal wall and your groin. Your surgeon will pull on the ends. This creates tension on your urethra that will help control urine. Tension may also help change the position of your urethra to keep your bladder from pressing on your urethra. Your surgeon may make other incisions in your lower abdomen to place a device to make adjustments to the sling later.
- Your surgeon will check for correct placement of the sling. A Foley catheter may be placed to help you urinate until swelling from surgery goes away. The incision may be closed with absorbable stitches or medical glue.
Purpose Of The Vaginal Sling Procedure
The vaginal sling procedure is one treatment option for stress urinary incontinence in women. Depending on how severe your urinary incontinence is, your doctor may prescribe other treatment options first. If those treatments dont work, your doctor may recommend the vaginal sling procedure. They may also recommend this procedure if you have a severe case of urinary incontinence and your bladder problems disrupt your everyday life.
The two main types of vaginal slings are conventional slings and tension-free slings.
Also Check: Benign Prostatic Hyperplasia With Urinary Obstruction
What Actions Has The Fda Taken
In 2008,the US Food and Drug Administration issued a Public Health Notification and Additional Patient Information that alerted healthcare providers and consumers about serious complications linked to the transvaginal placement of surgical mesh to treat pelvic organ prolapse and stress urinary incontinence .
The agency had received over 1,000 adverse event reports of complications arising from the use of mesh devices for POP and SUI repair. Most frequently reported complications include:
- Mesh erosion
- Dyspareunia
- Organ perforation
Years later, on July 2011, the FDA issued an update noting that serious complications associated with transvaginal mesh surgery for POP are not rare. The agency added that it is not clear whether transvaginal POP repair using mesh is more effective than traditional non-mesh repair.
Donât Miss: What Does The Start Of A Bladder Infection Feel Like
What Is A Male Sling Procedure
Urinary incontinence in men is common enough that there have been many methods of control developed. Adult diapers and various medications have been utilized by men suffering from all types of urinary incontinence. And if you are suffering from the same condition, it is safe to assume that you have considered these temporary solutions as a way to deal with your condition. But a procedure known as a male sling procedure could be the key to regaining your control permanently.
But what is a male sling procedure? How does it work? And what are the chances it can help you? OurSouth Florida urology specialists, with experience in all things urology from erectile dysfunction to silicone penis enlargement, are ready to answer these questions for you. But first, lets review the condition that started this search for treatment.
Read Also: Kidney Stone Vs Urinary Tract Infection
You May Like: Is Green Tea Good For Urinary Tract Infections
What Happens Before The Male Sling Procedure
Before surgery, you may be asked to see your family physician or anesthesiologist for a preoperative checkup. If necessary, your doctor will do a few tests. These tests could include:
- Urine tests
You may also be asked to follow a few rules before surgery. These include:
- Do not take Aspirin or any blood thinning medications two weeks before surgery. This includes medications such as ibuprofen naproxen and clopidogrel . If necessary, you can take Tylenol® for headaches or pain. Any other medication such as antibiotics, high blood pressure medications, hormone pills, and heart medications should be continued unless otherwise specified.
- Only consume clear liquids the night before surgery. This means anything you can see through, such as broth, juices and Jell-O. This helps keep the bowel clean at the time of surgery and reduces the risks of contamination.
- Do not eat or drink anything after midnight the day before surgery. Any medication that must be taken the morning of surgery should be taken with a small sip of water.
Is This The Right Urology Surgery For You
What is a male sling procedure? It can be simplified as follows: a tape that is similar to mesh in consistency and texture is placed in a problem area of the urethra. This action allows for the urethra to move into a new place, a new place that grants the patient control over their bladder once again. If it seems straightforward, its because it is.
A male sling procedure typically takes roughly 90 minutes to complete, and it is recommended that about 60 days be taken to fully recover with no strenuous activities like weightlifting occurring during that time period. The success rate for this procedure is said to range between 70-80%. Be sure to maximize the chances of success by going to a urology clinic that specializes in all types of male urology surgery.
Also Check: Do Probiotics Help With Urinary Tract Infections
What Should Women Do If They Have Concerns
Drs. Harmanli and Rickey say they have received numerous phone calls from past and current patients anxious about the news they have been hearing about pelvic mesh. If a woman was treated transvaginally with mesh for pelvic organ prolapse and has no complaints, she shouldnt worry and does not need to take any action, Dr. Harmanli says.
The word mesh shouldnt scare women, Dr. Rickey adds. There are other options to treat these disorders, and mesh is but one tool in a tool box with many others. Any treatment is a shared decision between doctor and patient, and we discuss the benefits and risks very carefully.
For What Procedures In Women Are Surgical Mesh Typically Used
Surgical mesh may be used to help repair pelvic organ prolapse and stress urinary incontinence in women.
In pelvic organ prolapse, the pelvic organs may shift downward and bulge out of the vagina. This occurs in women whose pelvic floor muscles and tissue are too weak to hold the organs in place.
Pelvic organs that may be subject to a prolapse include the bladder, uterus, rectum, vagina and urethra. Factors that can increase the chance of POP in women include pregnancy, childbirth and aging. The bladder is most often involved in pelvic organ prolapse. Prolapse of the bladder is called cystocele.
In stress urinary incontinence certain activities that increase pressure on the abdomen can cause urine to leak. These activities can include coughing, laughing, sneezing or exercising. The weakening of the pelvic muscles and tissues causes the bladder neck to move downward. As with pelvic organ prolapse, factors such as pregnancy, childbirth and aging may cause the pelvic muscles to stretch or weaken.
Also Check: How Do You Get An E Coli Urinary Tract Infection
A Briefhistory Of Mesh: Slings Vs Transvaginal
Inthe aftermath of the FDA ruling, mesh has become a four-letter word to most patients.But its important to remembernot all procedures that employ surgical mesh are created equal.
The FDA ban only applies to transvaginal mesh for prolapse repairs, which means there are still safe surgical options for treating POP and incontinence. These include:
- Bladder orvaginal slings: Theyve been around since the 1990s and are still consideredthe gold standard for treatment for stress urinary incontinence. Made of synthetic mesh or humantissue, the sling acts like a hammock around the urethra, preventing it fromopening during stresses on the bladder, like a laugh or a sneeze. Its placedthrough a small incision in the vagina and for women worried about leaking, its an effective option. Mostimportantly, the FDA did not ban bladder or vaginal mesh slings and it isendorsed by most female urology specialists and urogynecologists.