Causes Of Overflow Incontinence
Overflow incontinence, also called chronic urinary retention, is often caused by a blockage or obstruction to your bladder. Your bladder may fill up as usual, but as it is obstructed you will not be able to empty it completely, even when you try.
At the same time, pressure from the urine that is still in your bladder builds up behind the obstruction, causing frequent leaks.
Your bladder can become obstructed as a result of:
- an enlarged prostate gland
- bladder stones
- constipation
Overflow incontinence may also be caused by your detrusor muscle not fully contracting, which means that your bladder does not completely empty when you go to the toilet. As a result, the bladder becomes stretched. Your detrusor muscles may not fully contract if:
- there is damage to your nerves, for example as a result of surgery to part of your bowel or a spinal cord injury
- you are taking certain medications
Colposuspension And Sling Procedures
Aetna considers colposuspension and conventional suburethral sling procedures medically necessary for persons with stress UI that is refractory to conservative management .
Aetna considers adjustable retropubic suburethral sling in the treatment of stress urinary incontinence experimental and investigational because its effectiveness has not been established.
Aetna considers the colposuspension and suburethral sling procedures experimental and investigational for other indications because their effectiveness for indications other than the one listed above has not been established.
The Icd Code N394 Is Used To Code Overactive Bladder
Overactive bladder , also known as overactive bladder syndrome, is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person’s life. The frequent need to urinate may occur during the day, at night, or both. If there is loss of bladder control then it is known as urge incontinence. More than 40% of people with overactive bladder have incontinence. While about 40% to 70% of urinary incontinence is due to overactive bladder, it is not life-threatening. Most people with the condition have problems for years.
| Specialty: |
Recommended Reading: How To Clean Out Urinary Tract
Signs Of Urinary Incontinence
Urinary incontinence is not a disease in itself, but it can be a symptom of an underlying problem. The kind of symptoms you have will help determine the type of urinary incontinence.
Some symptoms may include:
Many people live with urinary incontinence, but it may affect your quality of life. You may feel embarrassed or worried about being too far from a restroom. You may also feel like you cant do normal daily activities or enjoy life. These are common feelings, which may indicate its time to talk to your doctor about how to manage your symptoms.
Causes Of Urge Incontinence
The urgent and frequent need to pass urine can be caused by a problem with the detrusor muscle in the wall of the bladder. The detrusor muscles relax to allow the bladder to fill with urine, then contract when you go to the toilet to let the urine out.
Sometimes the detrusor muscle contract too often, creating an urgent need to go to the toilet. This is known as having an ‘overactive bladder’. The reason your detrusor muscle contracts too often may not be clear, but possible causes include:
- drinking too much alcohol or caffeine
- poor fluid intake this can cause strong, concentrated urine to collect in your bladder, which can irritate your bladder and cause symptoms of overactivity
- conditions affecting the lower urinary tract , such as urinary tract infections or tumours in the bladder
- neurological conditions
- certain medications
Also Check: Food And Drink For Urinary Tract Infection
Causes Of Total Incontinence
Total incontinence occurs when your bladder cannot store any urine at all. It can result in you either passing large amounts of urine constantly, or passing urine occasionally with frequent leaking.
Total incontinence can be caused by:
- a problem with your bladder from birth
- injury to your spinal cord, which can disrupt the nerve signals between your brain and your bladder
- a bladder fistula, which is a small tunnel-like hole that can form between the bladder and a nearby area, such as the vagina, in women
Symptoms Of Urinary Incontinence
Having urinary incontinence means you pass urine unintentionally.
When and how this happens varies depending on the type of urinary incontinence you have.
Although you may feel embarrassed about seeking help, it’s a good idea to see your GP if you have any type of urinary incontinence.
Urinary incontinence is a common problem and seeing your GP can be the first step towards finding a way to effectively manage the problem.
Read Also: Will Az Pack Help A Urinary Tract Infection
What Treatment Is Available For Urinary Incontinence
Treatment for urinary incontinence depends on what type it is and whats triggering it, as well as your age, your overall health and medical history, how well you can tolerate medicines or therapies, and other factors. Your physician will take all this into account when prescribing a course of action.
Among the approaches available are special exercises, biofeedback, bladder training, vaginal weight training, pelvic floor electrical stimulation, and surgery.
- Behavioral therapies
- Bladder training teaches people to resist the urge to urinate and to gradually extend the intervals between visits to the toilet.
- Toileting assistance uses routine or scheduled toileting, habit-training schedules, and prompted voiding to empty the bladder regularly to prevent leaking.
Interstim Continence Control Therapy / Sacral Nerve Stimulation
You May Like: Can A Urinary Tract Infection Cause Diarrhea
Stress Urinary Incontinence / Prolapse
Interstim Continence Control Therapy/sacral Nerve Stimulation
Aetna considers implantation of the InterStim , a device for unilateral stimulation of the sacral nerve, medically necessary for the treatment of urge UI or symptoms of urge-frequency when all of the following criteria are met:
A test stimulation of the device is considered medically necessary for members who meet selection criteria 1 and 2 above.
Aetna also considers implantation of the InterStim medically necessary for the treatment of non-obstructive urinary retention when all of the following criteria are met:
Aetna considers removal of an Interstim medically necessary even where the initial implantation of the Interstim was not indicated.
According to the product labeling, InterStim therapy is contraindicated and has no proven value for individuals who have not demonstrated an appropriate response to test stimulation or are unable to operate the neurostimulator.
Exclusions
Recommended Reading: Over The Counter Urinary Tract Infection Medicine
Other Experimental And Investigational Interventions For Urinary Incontinence
Pelvic Floor Muscle Training
Your pelvic floor muscles are the muscles you use to control the flow of urine as you urinate. They surround the bladder and urethra .
Weak or damaged pelvic floor muscles can cause urinary incontinence, so exercising these muscles is often recommended.
Your GP may refer you to a specialist to start a programme of pelvic floor muscle training.
Your specialist will assess whether you are able to squeeze your pelvic floor muscles and by how much. If you can contract your pelvic floor muscles, you will be given an individual exercise programme based on your assessment.
Your programme should include doing a minimum of eight muscle contractions at least three times a day and doing the recommended exercises for at least three months. If the exercises are helping after this time, you can keep on doing them.
Research suggests that women who complete pelvic floor muscle training experience fewer leaking episodes and report a better quality of life.
In men, some studies have shown that pelvic floor muscle training can reduce urinary incontinence particularly after surgery to remove the prostate gland.
For more information:
- Pelvic, Obstetric and Gynaecology Physiotherapy : The Pelvic Floor Mucles – a Guide for Women
Recommended Reading: Sphincter Surgery For Urinary Incontinence
Posterior Tibial Nerve Stimulation
Your posterior tibial nerve runs down your leg to your ankle. It contains nerve fibres that start from the same place as nerves that run to your bladder and pelvic floor. It is thought that stimulating the tibial nerve will affect these other nerves and help control bladder symptoms, such as the urge to pass urine.
During the procedure, a very thin needle is inserted through the skin of your ankle and a mild electric current is sent through it, causing a tingling feeling and causing your foot to move. You may need 12 sessions of stimulation, each lasting around half an hour, one week apart.
Some studies have shown that this treatment can offer relief from OAB and urge incontinence for some people, although there is not yet enough evidence to recommend tibial nerve stimulation as a routine treatment.
Tibial nerve stimulation is only recommended in a few cases where urge incontinence has not improved with medication and you don’t want to have botulinum toxin A injections or sacral nerve stimulation.
Risk Factors & Diagnosis
Individuals are more likely to experience daytime incontinence if there is a family history. Multiple studies have found a strong heritable link particularly with nocturnal enuresis. This raises the age-old problem of nature versus nurture i.e. is it learnt or genetic? Daytime wetting is also more common in females and in individuals from low socioeconomic backgrounds and/or poor education. School is considered a risk factor due to restricted toilet times. Additionally, potentially embarrassing situations amongst peer groups may have an influence and also bad hygiene on school toilets. Some diseases such as childhood obesity and joint hypermobility are additionally considered to be a risk factor for daytime wetting. Children who have attention deficit hyperactive disorder are more likely to present with daytime incontinence and require more attentive treatment. Previously it was assumed that emotional/behavioural problems were causative of daytime wetting. This long-held belief is now being challenged and any associated behavioural problems in sufferers are more likely a response to incontinence.
You May Like: Physical Therapy For Urinary Incontinence
What Can I Do About Urinary Incontinence
If you are a woman with stress incontinence, you can help control your condition by doing Kegel exercises to make the muscles around the neck of the bladder stronger. To do this exercise, you squeeze the muscles you use to control the flow of urine, hold for up to 10 seconds, then release. Aim to do three sets of ten each day.
The best way to handle urge incontinence is to use the bathroom on a regular schedule. This might be a half-hour after a meal, two to three times between meals, and before going to bed.
Special products and equipment are available. Absorbent underwear, which is no more bulky than normal underwear, can be worn easily under everyday clothing. Incontinence may be managed by routinely inserting a catheter into the urethra and collecting the urine in a container.
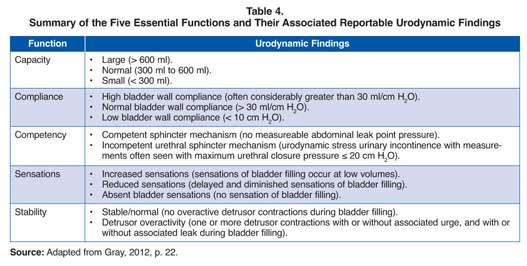
Bladder Structure And Function
The bladder, urethra and urinary sphincters work in concert to store urine at low pressure and to void voluntarily at socially convenient or appropriate times. The detrusor muscle and internal urethral sphincter are predominantly smooth muscle, whereas the external urethral sphincter and pelvic floor muscles are predominantly striated muscle. The bladder lumen is lined with epithelial cells and the basement membrane that protect the underlying detrusor muscle from toxins contained in the urine and enable communication with neural cells that coordinate storage and voiding phases .
Anatomy and histology of the female bladder
The sympathetic nervous system predominates during the storage phase and maintains continence through the paravertebral ganglia, the hypogastric nerves and hypogastric plexus. The parasympathetic system coordinates the voiding phase, through the sacral plexus and pelvic nerves . Afferent signals from the urothelium and bladder wall are transmitted through to the thalamus the balance between storage and voiding is maintained by the central pontine micturition centre . The neurotransmitters responsible for execution of these commands are acetylcholine and noradrenaline.
Neurological control of the urinary bladder
Also Check: What Is The Most Common Antibiotic For Urinary Tract Infection
Gene Testing For Stress Urinary Incontinence
An UpToDate review on Evaluation of women with urinary incontinence states that The risk of urinary incontinence, particularly urgency incontinence, may be higher in patients with a family history. One study found that the risk of incontinence was increased for both daughters and sisters of women with incontinence. Twin studies attribute a 35 to 55 % genetic contribution to urgency incontinence/overactive bladder but only 1.5 % for stress incontinence.
Furthermore, an UpToDate review on Urinary incontinence in men does not mention genetic testing as a management option.
Botulinum Toxin A Injections
Botulinum toxin A can be injected into the sides of your bladder to treat urge incontinence and overactive bladder syndrome .
This medication can sometimes help relieve these problems by relaxing your bladder. This effect can last for several months and the injections can be repeated if they help.
Although the symptoms of incontinence may improve after the injections, you may find it difficult to fully empty your bladder. If this happens, you will need to be taught how to insert a catheter into your urethra to drain the urine from your bladder.
Botulinum toxin A is not currently licensed to treat urge incontinence or OAB, so you should be made aware of any risks before deciding to have the treatment. The long-term effects of this treatment are not yet known.
Read Also: Urinary Tract Infection And Period
Care Of Persons With Stroke And Urinary Symptoms
UI in the setting of an acute stroke is associated with more severe functional limitations than those with acute stroke and no UI. Additionally, the ability to toilet independently is predictive of more positive rehabilitation outcomes such as improved quality of life, functional recovery, and remaining in community-dwelling . Persons with a history of cerebrovascular disease may be predisposed to urgency urinary symptoms or have symptoms of impaired sensory integration of bladder afferent signals. Patients may also report UI without sensory awareness. Patients who describe UI without sensory awareness may benefit from scheduled toileting, which can be personalized based on a bladder diary. Emptying the bladder every 23 h, regardless of the sensation to void, will help to maintain continence. Bladder relaxants may not reduce UI without sensory awareness unless other symptoms of OAB, such as daytime urinary frequency, are also present.