Alternative And Complementary Therapies
The treatment of urinary incontinence varies depending on the cause of the bladder control problem. In most cases, a physician will try the simplest treatment approach before resorting to medication or surgery.
Bladder habit training This is the first approach for treating most incontinence issues. The goal is to establish a regular urination schedule with set intervals between urination. A doctor will usually recommend urinating at one-hour intervals and gradually increasing the intervals between urination over time.
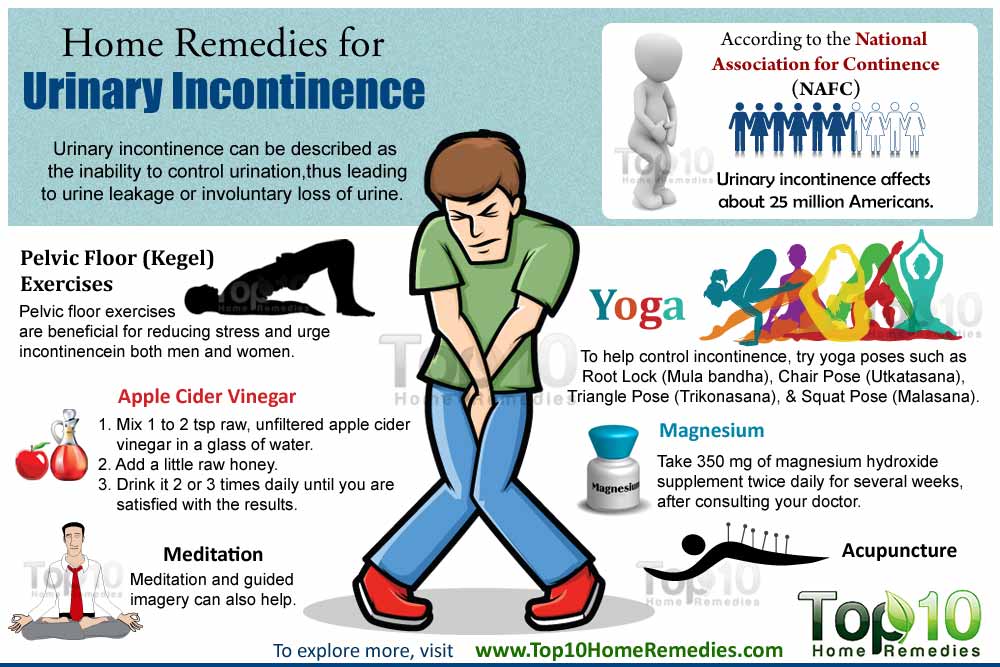
Pelvic muscle exercises Also called Kegel exercises , this exercise routine helps strengthen weak pelvic muscles and improve bladder control.
The person contracts the muscles used to keep in urine, holds the contraction for 4 to 10 seconds, then relaxes the muscles for the same amount of time.
It may take weeks or months of regular pelvic exercise to show improvement.
Another way to perform Kegel exercises is to interrupt the flow of urine for several seconds while urinating.
How Soon After Starting Kegel Exercises Will Urinary Incontinence Get Better
It may take 4 to 6 weeks before you notice any improvement in your symptoms.10
Kegel exercises work differently for each person. Your symptoms may go away totally, you may notice an improvement in your symptoms but still have some leakage, or you may not see any improvement at all. But even if your symptoms dont get better, Kegel exercises can help prevent your incontinence from getting worse.
You may need to continue doing Kegel exercises for the rest of your life. Even if your symptoms improve, urinary incontinence can come back if you stop doing the exercises.
Other Types Of Urinary Incontinence
- Overflow incontinence This occurs when a person is unable to empty their bladder completely and it overflows as new urine is produced. It’s often found in people with diabetes or spinal cord injuries.
- Mixed incontinence You show evidence of more than one type.
- Functional incontinence This type of incontinence has less to do with a bladder disorder and more to do with the logistics of getting to a bathroom in time. It’s usually found in elderly or disabled people who have normal or near normal bladder control but cannot get to the toilet in time because of mobility limitations or confusion.
- Nocturia The need to urinate twice or more during the night, usually affecting men and women over the age of 60. In men, nocturia can be a symptom of an enlarged prostate.
You May Like: Will Cranberry Juice Help A Urinary Tract Infection
Treatment Options For Stress Incontinence:
- Pelvic floor physical therapy This can improve up to 75% of symptoms.
- Pessary This device, inserted in the vagina, helps control leakage by providing support under the urethra and bladder.
- Urethra bulking This office-based procedure can help thicken the wall of your urethra so it more tightly seals to hold urine.
- Sling urethral surgery This outpatient surgery stops urine leakage via a sling that lifts and supports your urethra and lower bladder.
“If stress incontinence is severe, sling urethral surgery is typically about 95 percent successful and there’s very little down time as far as returning to everyday activities,” says Dr. Lindo.
What Is Bladder Training
Bladder training is a way of learning to manage urinary incontinence. It is generally used for stress incontinence, urge incontinence, or a combination of the 2 types .
Bladder training can help in the following ways:
- Lengthen the amount of time between bathroom trips
- Increase the amount of urine your bladder can hold
- Improve your control over the urge to urinate
Some bladder training techniques are explained in Bladder Training for Urinary Incontinence.
Read Also: Can Drinking Lots Of Water Cure A Urinary Tract Infection
If You Have Had Little Luck With Other Incontinence Interventions You May Need To Consider These Interventional Therapies:
- BotoxInjections of Botox into the bladder muscle may benefit you if you have an overactive bladder. Botox generally is prescribed only if medications or conservative treatments haven’t been successful.
- InterStim therapy With this therapy, a small device the size of a pacemaker is placed under the skin in your hip area. A lead wire is connected to the device and sends electrical impulses to the sacral nerves, which control bladder contraction and function.
- Percutaneous tibial nerve stimulation This therapy is designed to stimulate the nerves responsible for bladder control using the tibial nerve in your lower leg. During the procedure, a small, slim needle electrode is inserted near your tibial nerve and connected to a battery-powered stimulator. The impulses travel to the tibial nerve and then to the sacral nerve, which controls bladder control and function.
Watch this video to learn more about urinary incontinence treatments including sacral neuromodulation therapy:
Read more helpful tips and lifestyle changes that can help you manage urinary retention and incontinence.
For the safety of our patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a non-patient care area where social distancing and other safety protocols were followed.
Topics in this Post
Can Urinary Incontinence Be Prevented Or Avoided
You may be able to prevent urinary incontinence by working to keep pelvic muscles strong. But even so, it doesnt guarantee that you will never have urinary incontinence.
There are also lifestyle changes you can make to help prevent urinary incontinence. You may find it helpful to make some changes in your diet. Alcohol, caffeine, foods high in acid , and spicy foods can irritate your bladder. Talk to your doctor if you think your diet may contribute to your incontinence.
Some people find that limiting how much they drink before bedtime helps reduce nighttime incontinence.
Losing weight if you are overweight can also help reduce incontinence.
You May Like: How Does Someone Get A Urinary Tract Infection
Bladder Incontinence In Women
Bladder incontinence is more common in women than in men. Other than the possible causes listed above, some things that may increase risk of bladder incontinence in women are:
- Changes to urinary or vaginal tissue from hormone therapy, surgery, chemotherapy, or targeted therapy
- Hormonal changes from menopause
- Pelvic prolapse – the bladder, uterus, and or rectum may slip backward or downward into the vaginal canal because of weak pelvic wall muscles
- Pregnancy
- Hysterectomy
What Are The Treatments For Urinary Incontinence
Numerous treatment alternatives are accessible.
You May Like: Urinary Tract Infection Pills Over The Counter
How Is Incontinence Diagnosed
Often, the diagnosis process for incontinence will start with a conversation with your healthcare provider about your medical history and bladder control issues. Your provider might ask you questions like:
- How often do you urinate?
- Do you leak urine between trips to the toilet, how often does this happen and how much urine do you leak each time?
- How long have you been experiencing incontinence?
These questions can help your provider figure out a pattern with your leakage, which often points to a specific type of incontinence. When your provider is asking about your medical history, its important to list all of your medications because some medications can cause incontinence. Your provider will also ask about any past pregnancies and the details around each delivery.
There are also several specific tests that your provider might do to diagnose incontinence, including:
While at home, your provider might recommend you keep track of any leakage in a journal for a few days. By writing down how often you experience incontinence issues over the span of a few days, your provider might be able to identify a pattern. This can really help in the diagnosis process. Make sure to write down how often you need to urinate, how much you are able to go each time, if you leak between trips to the bathroom and any activities you might be doing when you leak urine. Youll then bring this journal with you to your appointment and talk about it with your provider.
Home Remedies For Utis
Along with antibiotic use, some individuals have found relief with:
Vitamin C.Studies suggest Vitamin C increases the acidity of the urine to kill off bacteria. Vitamin C can be found in fruits and vegetables like red peppers, oranges, and kiwis.
Probiotics. Probiotics can promote a healthy balance of bacteria in the gut with beneficial microorganisms. Lactobacillus is a common probiotic strain that has been linked to preventing UTIs. Probiotics are found in supplements, yogurt, kefir, and some cheeses.
Cranberry. Cranberry has also been shown to prevent urinary tract infections. Research shows that cranberry aids in preventing bacterial binding to host cell surface membranes in the urinary tract, limiting the ability for the bacteria to stick to the walls of the bladder, which causes infection. Concentrated cranberry capsules, as opposed to cranberry juice, are recommended. 300mg-400mg twice daily is the recommended dose.
Read Also: Is Azithromycin Good For Urinary Tract Infection
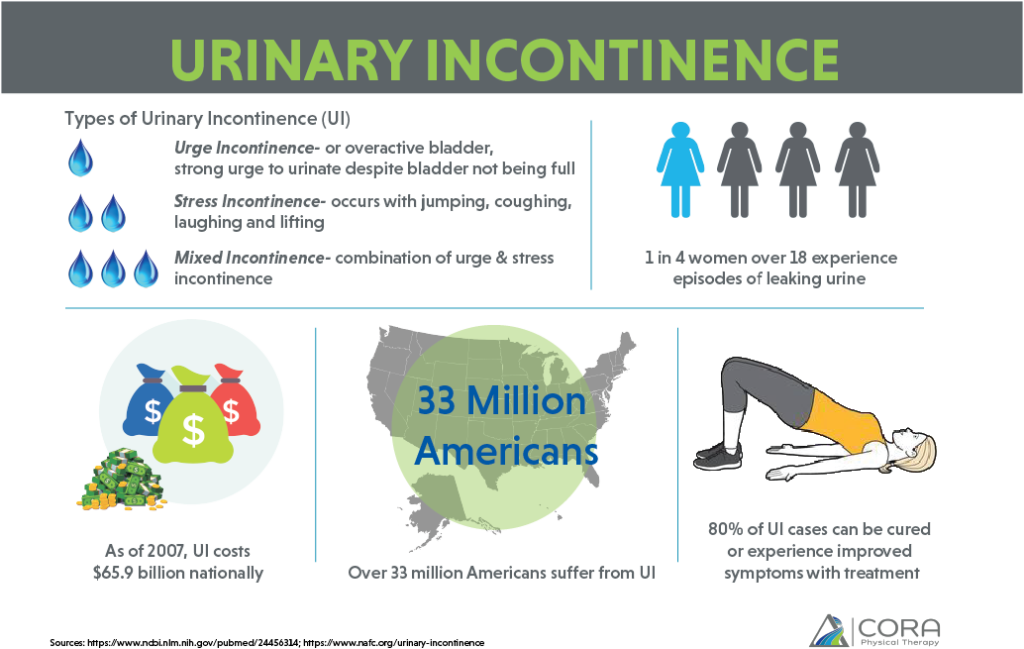
Types Of Urinary Incontinence
There are different types of incontinence:
- Stress incontinence occurs when urine leaks as pressure is put on the bladder, such as during exercise, coughing, sneezing, laughing, or lifting heavy objects. Its the most common type of bladder control problem in younger and middle-aged women. It also may begin later, around the time of menopause.
- Urge incontinence happens when people have a sudden need to urinate and cannot hold their urine long enough to get to the toilet. It may be a problem for people who have diabetes, Alzheimers disease, Parkinsons disease, multiple sclerosis, or stroke.
- Overflow incontinence happens when small amounts of urine leak from a bladder that is always full. A man can have trouble emptying his bladder if an enlarged prostate is blocking the urethra. Diabetes and spinal cord injuries can also cause this type of incontinence.
- Functional incontinence occurs in many older people who have normal bladder control. They just have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly.
Should I Drink Less Water Or Other Fluids If I Have Urinary Incontinence
No. Many people with urinary incontinence think they need to drink less to reduce how much urine leaks out. But you need fluids, especially water, for good health.
Women need 91 ounces of fluids a day from food and drinks.11 Getting enough fluids helps keep your kidneys and bladder healthy, prevents urinary tract infections, and prevents constipation, which may make urinary incontinence worse.
After age 60, people are less likely to get enough water, putting them at risk for dehydration and conditions that make urinary incontinence worse.12
Don’t Miss: I Have A Urinary Tract Infection
What Your Treatment Will Involve
Your healthcare professionals recommended treatment plan will depend on the cause of your incontinence. An underlying medical condition may require medication, surgery, or other treatments.
In certain situations, they may not be able to cure your bladder incontinence. In these cases, they will likely provide steps you can take to manage your condition.
Treatment options for urinary incontinence may include:
You cant prevent all cases of urinary incontinence, but there are steps you can take to reduce your risk of developing it.
For example, try to:
Controlling The Need To Urinate
Some activities may increase leakage for some people. Things to avoid include:
- Coughing, sneezing, and straining, and other actions that put extra pressure on the pelvic muscles. Get treatment for a cold or lung problems that make you cough or sneeze.
- Very heavy lifting.
Ask your provider about things you can do to ignore urges to pass urine. After a few weeks, you should leak urine less often.
Train your bladder to wait a longer time between trips to the toilet.
- Start by trying to hold off for 10 minutes. Slowly increase this waiting time to 20 minutes.
- Learn to relax and breathe slowly. You can also do something that takes your mind off your need to urinate.
- The goal is to learn to hold the urine for up to 4 hours.
Urinate at set times, even if you do not feel the urge. Schedule yourself to urinate every 2 to 4 hours.
Empty your bladder all the way. After you go once, go again a few minutes later.
Even though you are training your bladder to hold in urine for longer periods of time, you should still empty your bladder more often during times when you might leak. Set aside specific times to train your bladder. Urinate often enough at other times when you are not actively trying to train your bladder to help prevent incontinence.
Ask your provider about medicines that may help.
Surgery may be an option for you. Ask your provider if you would be a candidate.
Read Also: Does Azo Work For Urinary Tract Infections
The Proper Way To Kegel
Verbal or written instructions alone don’t necessarily help patients know whether they’re doing Kegel exercises properly.
When we see patients for urinary incontinence, we provide education and instruction. We often recommend one to six sessions of supervised Kegel exercises with a female pelvic medicine and reconstructive surgery doctor, a pelvic floor physical therapist, or another provider who has expertise in pelvic floor disorders. While physical therapy or other medical visits usually are not covered by insurance for preventive purposes, they usually are once a problem develops.
In these appointments, your provider will describe how to locate and engage the pelvic floor muscles. The provider will gently press on the pelvic floor muscles with a gloved exam finger inside your vagina and ask you to squeeze the muscles. The muscles will be identified as described. Make sure youre not squeezing your stomach, legs, or gluteal muscles at the same time, and dont hold your breath.
Some patients benefit from holding a mirror between the legs to visualize the external anatomy during the exercise. When done properly, you should see the area between your vagina and anus lift toward your upper body.
Doing Kegel exercises regularly is key to strengthening the pelvic floor. We recommend women do 10 repetitions, holding each squeeze for 5 to 10 seconds, three times each day.
Tips For Living With Urinary Incontinence
With a little planning, you can manage your urinary incontinence so it doesnt affect your life too much. There are many products available to help you live with incontinence, such as pads, catheters or bedding protection. Some of these are subsidised by the government.
It can help to get into a routine. Plan for outings, make sure you have enough products and spare clothes in case you have an accident, and know how to find the nearest toilet.
Other tips include:
- Avoiding lifting. Lifting puts strain on your pelvic floor muscles, so avoid it wherever you can. When you do need to lift something, such as when picking up children or shopping bags, tighten your pelvic floor muscles before and during the lift.
- Drinking plenty of water. Many people with urinary incontinence avoid drinking fluids as they feel it causes more problems. However, limiting your fluid intake makes incontinence worse because it reduces your bladder’s capacity. Some medical conditions may require you to limit your fluid intake, so ask your doctor if youre unsure how much water you should drink each day.
- Avoiding certain foods. Spicy and acidic foods, such as curries and citrus fruits, can irritate the bladder and make symptoms worse.
- Download the National Public Toilet Map, which shows the location of more than 19,000 public and private public toilet facilities across Australia.
Don’t Miss: Urinary Tract Infection Otc Antibiotics
Good Toilet Habits Help Prevent Incontinence
Good toilet habits can help to prevent bladder and bowel problems. Suggestions include:
- Go to the toilet to urinate only when your bladder is full. If you make a habit of trying to urinate just in case, youll teach your bladder to signal the urge to urinate when it isnt full.
- Take your time on the toilet. Allow urine to flow at its own speed .
- Go to the toilet when you feel the urge to pass a bowel motion. Hanging on can lead to constipation.
- Give yourself plenty of time to pass a bowel motion.
- Dont strain to open your bowels. Regular straining can cause problems including haemorrhoids , and can weaken your pelvic floor muscles.
- Use correct posture on the toilet . Put your feet on a footstool, place your elbows on your knees, bulge out your stomach and straighten your back.
- Treat laxatives as a short-term solution and work on treating constipation with diet, exercise and lifestyle changes.
Drink Plenty Of Water
Drink 6 to 8 glasses of fluid a day unless your doctor advises you otherwise.
Many people with urinary incontinence avoid drinking fluids, as they feel it causes more problems. However, limiting your fluid intake makes incontinence worse, because it reduces your bladder’s capacity.
Not drinking enough fluid can also cause constipation or make it worse.
Find out which are the healthiest drinks.
Don’t Miss: How To Strengthen Urinary Sphincter