Reasons To Have Prostate Surgery
One of the most common reasons for having prostate surgery, or a prostatectomy, is to treat prostate cancer.
According to the American Cancer Society, prostate cancer is the second most common form of cancer in American men, right behind skin cancer. Nearly 174,000 new cases are reported in the United States every year. If the cancer has not yet spread outside of the prostate gland, then surgery will be a great treatment option. Another reason to have prostate surgery is to treat an enlarged prostate.
As the prostate grows, it may block the flow of urine which can create bladder, urinary tract, and kidney related problems. Removing a part of the prostate can help to solve or prevent these issues.
You May Like: Is Prostate Cancer Genetically Inherited
The Long Wet Road Back To Normal
Incontinence after radical prostatectomy sucks. But for nearly all men, it goes away. For the very small percentage in whom it doesnt, there is help.
JP Mac is an Emmy award-winning animation writer who worked for Warner Bros. and Disney, and a novelist. He is also very funny.
So, when he wrote a short ebook about his experience with prostate cancer including his diagnosis in 2014 at age 61, the rush to find the right treatment and get it done before his health insurance was going to expire, his laparoscopic-robotic prostatectomy and the complications afterward, and his five-month battle to recover urinary continence after the surgery he could legitimately have written a soap opera, or maybe even a tear-jerker but he didnt.
Instead, his ebook has a title that sounds like 1950s pulp fiction: They Took My Prostate: Cancer, Loss, Hope. Its not Prostate Cancer Lite, and it doesnt minimize what he or anyone else has gone through to get back to normal after radical prostatectomy. Far from it in fact, his short, hopeful essay is a testament to what it takes to recover from this difficult but life-saving surgery: a balanced perspective, a good sense of humor, a great support system, and plain old hard work and persistence.
Heres a message you hardly ever hear about prostate cancer, or any illness, for that matter: Its okay to laugh! That doesnt mean its not scary, and that it doesnt wear you down, or that youre not afraid you wont ever get back to normal.
Why Prostate Laser Surgery
Compared to open prostatectomy and transurethral resection of the prostate, prostate laser surgery offers significant advantages to the patient. They include a general lower risk of post-surgery bleeding, a much shorter hospital stay , and a much quicker recovery. Men who undergo prostate laser surgery for BPH will also, in contrast to other procedures, generally notice an improvement in their urinary output and comfort right away. They are highly unlikely to need a urinary catheter for longer than 24 hours, again unlike with other procedures.
Long-term complications are also much less likely with prostate laser surgery than with more traditional forms of prostate surgery. Though that is good news, laser prostate surgery still carries both short-term and long-term risks, just like practically any other surgery. What are they?
Also Check: Urinary Tract Infection Immediate Relief
How Long Does It Take To Overcome Incontinence After Undergoing Prostate Cancer Surgery
A study showed that 88% of post-prostatectomy patients suffering from stress incontinence were still suffering up to 1-year later1.
However, as Post Prostate Cancer Surgery patients will experience different degrees of side effects, so do they recover from these side effects at variable rates. In most cases, the recovery time for Urinary Incontinence Post Prostate cancer surgery ranges from 6-12months in most cases2, with continence improving progressively up until 2 years post-surgery2.
Why Does It Happen
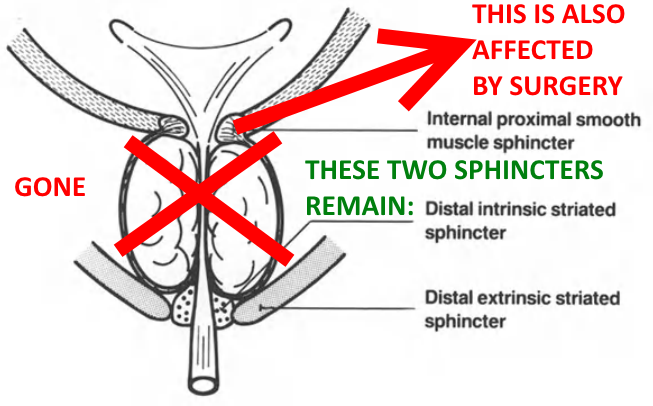
- At the point where the bladder and urethra join, there is a ring of muscles known as the bladder neck sphincter, which opens and closes like a camera shutter. The bladder neck sphincter is closed most of the time to prevent urine leaking out, but when it gets a signal from the brain, it opens to allow urine to be passed.
- If the bladder neck sphincter is damaged during prostate cancer surgery, this can lead to urinary incontinence.
- Another sphincter is part of another set of muscles below the prostate called the pelvic floor. These muscles are also involved in bladder control.
Most men regain their bladder control over time and are fully recovered within 6 to 12 months. It is important to get professional advice to help cope bladder weakness during this time.
Recommended Reading: How Does Botox Work For Urinary Incontinence
Urinary Problems After Prostate Cancer Treatment
Many men get urinary problems as a side effect of their treatment. This is because prostate cancer treatment can damage the nerves and muscles that control when you urinate .
If youre starting treatment for prostate cancer, ask your doctor about the possible side effects. Each treatment can cause different urinary problems. Your chances of getting each side effect will depend on the treatment youre having, and on whether or not you had urinary problems before starting treatment.
If youve already had prostate cancer treatment and you have urinary problems, tell your doctor or nurse. They can suggest treatments and lifestyle changes to help manage them.
Depending on the type of problems youre having, ways to manage them can include lifestyle changes, pelvic floor muscle exercises, bladder retraining, medicines or surgery. For practical tips read our How to manage urinary problems guide.
Watch Paul’s story below for one man’s experience of managing urinary problems after prostate cancer treatment.
Exercise Your Pelvic Floor Muscles
Learning how to control the pelvic floor muscles can speed up the recovery process and reduce leakage. If you dont strengthen these muscles, the leakage may persist.
Please note: Performing pelvic floor muscle exercises before and after prostate surgery is vital to your recovery. Resume pelvic floor exercises once the catheter has been removed to avoid bladder irritation and discomfort. It is recommended that you seek help from a mens, womens and pelvic health physiotherapist, Nurse Continence Specialist, or urology nurse to learn the correct technique.
More information about the pelvic floor muscles can be found on our pelvic floor and male pelvic floor pages. You can also learn more about pelvic floor friendly exercises at pelvicfloorfirst.org.au.
Also Check: Amoxicillin For Urinary Tract Infection
Don’t Miss: Urinary Tract Infection In Men Homeopathic Treatment
The Procedure That Got Me Dry Again After Nine Years Of Incontinence
Like many men, Peter Barton had to deal with urinary incontinence after prostate surgery and was among those who dont see the problem improve over time. After years of using pads as the problem got worse, Peter decided to try a surgical treatment the male sling.
PETER: As a fit farmer aged 65 it was a great shock when I was diagnosed with prostate cancer back in 2008. My wife and I examined all the options for treatment and opted for robotic assisted surgery, which was then still in its early development in the UK.
The surgery went well. My excellent urologist had said that wed just got the tumour before it had broken out of the prostate and my family were much relieved as he confirmed the cancer was unlikely to return.
I was out of hospital in two days but had to wear a catheter for two weeks these were pretty miserable weeks. It wasnt painful at all, but it was awkward. It kept getting caught up on things and was constantly leaking. Things improved when the catheter was removed however I was left incontinent.
For the next nine years life was good but, although I followed instructions about pelvic floor exercises, which I know work for some men, my incontinence slowly worsened. For the first year or two I was using a size one pad the lightest. After two years, Id moved on to the number two and by the last few years I was on a number three, which needed changing several times a day. Each of these can hold a considerable amount of urine.
Epidemiology And Natural History Of Urinary Incontinence After Rp
RP, regardless of approach, leads to changes in urinary function, including urinary incontinence, that usually resolve by the end of the first postoperative year. The rate of urinary incontinence after RP depends on the definition of urinary incontinence and the methodology used to collect the data.24 Walsh and colleagues5 assessed the continence rate at 10 years in their first 593 patients undergoing the anatomic nerve-sparing RP. They reported that 6% wore 1 or fewer pads per day. No patient was reported as being totally incontinent. Catalona and Basler6 reviewed their series of 435 men undergoing nerve-sparing RP and found that, with a minimum of 18-month follow-up, 409 were continent. They defined continence as not needing pads and occasionally leaking 1 or 2 drops of urine with severe abdominal straining. Eastham and associates,2 in reviewing continence results after RP, defined continence as those patients who did not use pads or who used a pad occasionally although they were consistently dry with moderate exercise those who leaked urine onto 1 or more pads daily with moderate exercise were considered to have stress urinary incontinence , and those who were wet with normal activity were considered severely incontinent. The authors reported a continence rate of 91% at 2 years after RP.
Most men have incontinence immediately after RP. Recovery of urinary continence can take up to 1 year, with a small minority of patients recovering continence up to 3 years after RP.10
Recommended Reading: Prescription Drugs For Urinary Tract Infection
What Causes Incontinence After Prostate Surgery
Urinary incontinence is a potential side effect of prostate removal surgery. The prostate is located just below the bladder and surrounds the urethra. Removing it , or using radiation to treat it, can sometimes cause damage to the nerves and muscles of the bladder, urethra, and or sphincter, which controls the passage of urine from the bladder. This can result in urinary incontinence. In this instance, men are usually experiencing stress urinary incontinence, which is a type of incontinence that happens when you place increased pressure on the bladder. Things like sneezing, coughing, working out, and even standing up can cause you to leak urine.
Surgery To Treat Urinary Incontinence
For patients with urinary incontinence that is not improving, your doctor may recommend treatments such as an artificial urinary sphincter or a urethral sling. An artificial urinary sphincter involves the surgical implantation of a device around the urethra that controls your urine. When the sphincter is closed, it blocks the passage of urine that may leak from your bladder. It is controlled by a pump, which you squeeze when you want to urinate.
A urethral sling is also placed around your urethra, and it provides added support to the urethra to prevent urine leakage. The sling will lift the urethra and add pressure to it to help with urine retention.
Also Check: What Are The Symptoms Of Urinary Tract Infection In Males
Is It Possible To Treat Urinary Incontinence After A Prostate Surgery
Professionals suggest noninvasive surgeries and muscle strengthening exercises for the pelvis if the problems persist. These therapies and solutions help reduce the number of times you need to go to the bathroom to urinate. However, this solution works best for people who have mild symptoms.
Patients who cannot stop urine from leaking may need surgery besides using pads, incontinence wipes, or similar products for the problem. Let us take a look at these solutions in detail.
Oab And Urgency Incontinence
In the context of management of post-rPR OAB syndrome, it is important to understand its underlying pathophysiological mechanism . Since OAB is multifactorial , the exact role of prostate surgery in the development of OAB is still under debate as, after rPR, there are several variables that could contribute to detrusor overactivity.
Detrusor overactivity in patients after radical prostatectomy has been mainly attributed to a partial denervation of the bladder during surgery . However, together with bladder denervation, other hypotheses, such as the urethrovesical mechanism, have been described.
It has been demonstrated that urethral afferents are activated by urethral perfusion and they could modulate the micturition reflex via pudendal and pelvic afferent and efferent signals, causing bladder contraction. This has been described as urethrovesical mechanism .
In a recent study, Mastukawa et al. identified that low maximum urethral closure pressure at baseline and its decrease postoperatively were strong predictors of de novo post-rPR OAB underlying the role of the intrinsic sphincter deficiency on the pathophysiology of OAB .
In contrast, detrusor underactivity may cause OAB syndrome as well, which seems contradictory at the first glance. Bladder underactivity may affect up to 40% of patients after radical prostatectomy mostly due to denervation .
Also Check: Symptoms Of Pinworms In Urinary Tract
What Is The Prostate
The prostate is part of a mans sex organs. Its about the size of a walnut and surrounds the tube called the urethra, located just below the bladder.
The urethra has two jobs: to carry urine from the bladder when you urinate and to carry semen during a sexual climax, or ejaculation. Semen is a combination of sperm plus fluid that the prostate adds.
How Does The Smart Technique Spare The Urinary Function
Employing the da Vinci System, he uses his own SMART to remove the prostate and spare urinary and sexual functions. At the beginning of surgery, Dr. Samadi does not suture the dorsal vein complex, allowing him to control the length of the urethra. The more urethra he can leave, the less incontinence and leaking a man will experience after surgery. Further, with robotic surgery a catheter is only needed for roughly one week following surgery, so the patient is more comfortable and there is less trauma to normal urinary function. Sexual performance is also preserved because Dr. Samadi does not open the endopelvic fascia during surgery. Leaving this tissue intact spares the nerve bundles that control sexual function.
A study was published on this subject, explaining urinary incontinence after prostate surgery.
It is important to accept that most men will experience some degree of urinary incontinence after prostate surgery. This is not an indication of long-term damage. Regaining urinary control can take several weeks or months and some men dont reach their full recovery capacity for a year or more. Age, weight and previous urinary issues are also factors in recovery time. Patients of Dr. Samadis who experienced normal continence prior to surgery can expect to regain urinary control within 12 to 13 months.
Don’t Miss: Can Clarithromycin Be Used To Treat A Urinary Tract Infection
Who Is At Risk For Developing Incontinence
It is not known why some men have incontinence that continues after surgery and others do not. SUI after surgery could be caused by::
- Older age.
- Larger prostate size before its removal.
- Smoking.
- Diabetes or other neurological diseases.
- A lot of blood loss during surgery.
- Need for cutting nerves during surgery.
- Size or stage of prostate tumor.
- Radiation after surgery .
- Previous surgery for BPH.
Radical Prostatectomy Retropubic Or Suprapubic Approach
Youll be positioned on the operating table, lying on your back.
An incision will be made from below the navel to the pubic region.
The doctor will usually perform a lymph node dissection first. The nerve bundles will be released carefully from the prostate gland and the urethra will be identified. The seminal vesicles may also be removed if necessary.
The prostate gland will be removed.
A drain will be inserted, usually in the right lower area of the incision.
You May Like: Urinary Tract Infection Kidney Pain
Risk Of Bias Assessment
The Newcastle Ottawa scale, which evaluates cohort selection, comparability and outcomes assessment, was used for non-randomized controlled trials . The Cochrane risk of bias tool which evaluates random sequence generation, allocation concealment, blinding, and attrition was used for evaluation of RCTs.
Read Also: Severe Urinary Tract Infection Symptoms In Elderly
Do Laser Treatments Have Any Advantages Over Turp
As well as the standard approaches such as TURP, there are a number of other surgical techniques. They mainly differ in terms of the instruments and sources of energy used to remove or destroy the prostate tissue. Most of the other techniques are carried out using laser beams. Like in TURP, the instruments are inserted into the urethra and guided to the prostate.
The laser treatments include:
- Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med 1995 332: 75-79.
-
IQWiG health information is written with the aim of helpingpeople understand the advantages and disadvantages of the main treatment options and healthcare services.
Because IQWiG is a German institute, some of the information provided here is specific to theGerman health care system. The suitability of any of the described options in an individualcase can be determined by talking to a doctor. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by ateam ofhealth care professionals, scientists and editors, and reviewed by external experts. You canfind a detailed description of how our health information is produced and updated inour methods.
Don’t Miss: Foods That Cause Urinary Tract Infections
I Had No Idea What Bladder Spasms Were
I had never heard of bladder spasms before. According to WebMD, a persons bladder normally fills up with urine and gradually you feel the need to urinate. But with a bladder spasm, the bladder contracts suddenly and involuntarily, and that urge to go is immediate, overwhelming, and sometimes painful. Bladder spasms are common after surgery, and can be an unhappy consequence of having a catheter, which I would for the three weeks after surgery.
But at the time of my discharge, I knew none of this. I was told that the painkiller and bladder relaxant were just in case I had bladder spasms, and that they could hurt a little, if I got them at all. What I did not realize was that the bladder relaxant kept spasms from happening in the first place, and that they are incredibly common with a catheter in place. So I pocketed the latter two prescriptions and hoped I wouldnt get a bladder spasm whatever those were.
Unfortunately, I did.