Diseases Of The Genitourinary Systemtype 2 Excludes
What Is The Icd 10 Code For Incontinence
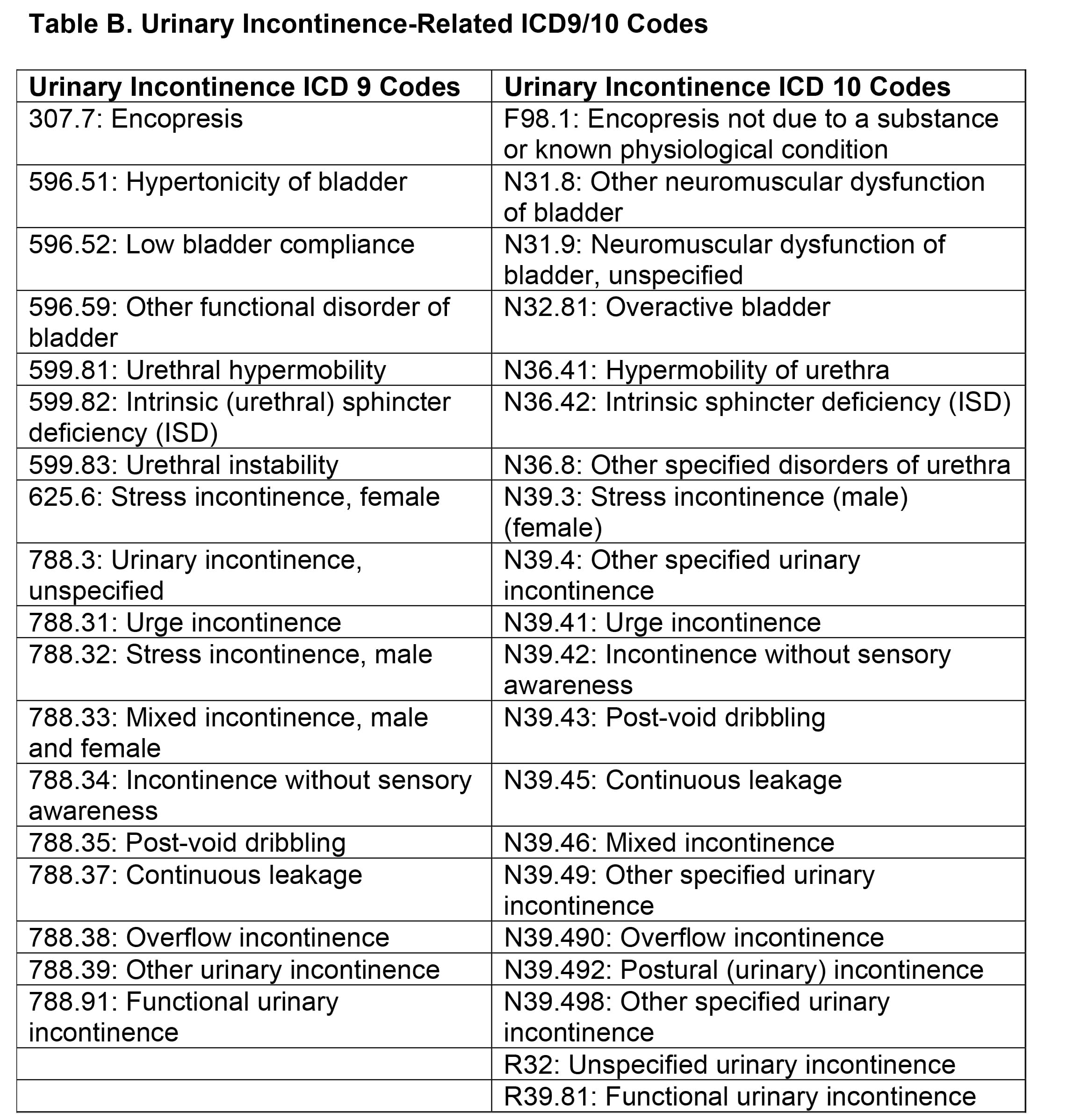
N39.42 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM N39. 42 became effective on October 1, 2021.
How do you code urinary incontinence?
2022 ICD-10-CM Diagnosis Code R39.81: Functional urinary incontinence.
What is diagnosis code N39 46?
2022 ICD-10-CM Diagnosis Code N39. 46: Mixed incontinence.
What is the ICD 10 code for mixed stress and urge urinary incontinence?
What is diagnosis code R32?
R32: Unspecified urinary incontinence.
Magnetic Stimulation For Women With Stress Urinary Incontinence
In a meta-analysis of studies with short-term follow-up, Peng and colleagues examined the efficacy of magnetic stimulation in female patients with SUI by investigating peer-reviewed RCTs. PubMed, Embase, and Cochrane library were retrieved for any peer-reviewed original articles in English. Databases were searched up to July 2018. Included studies examined effects of MS on SUI. The data were analyzed by review manager 5.3 software . A total of 4 studies involving 232 patients were identified and included in present meta-analysis. Compared with the sham stimulation, the MS group had statistically significantly fewer leaks/3 days , less urine loss on pad test , higher QoL scores , and lower ICIQ scores . MS presented higher cure or improvement rate, with a statistically significant improvement in UDI and IIQ-SF scores compared to sham stimulation. No MS-related AEs were reported in study. The authors concluded that MS led to an improvement in SUI without any reported safety concerns and an improvement in patient QoL however, the long-term outcome of this technique remains unclear and is the subject of ongoing research.
Recommended Reading: Urinary Incontinence Causes In Females
How Do You Code Cva And Hemiparesis In Sequela
Coding Guidelines
Residual neurological effects of a stroke or cerebrovascular accident should be documented using CPT category I69 codes indicating sequelae of cerebrovascular disease. Codes I60-67 specify hemiplegia, hemiparesis, and monoplegia and identify whether the dominant or nondominant side is affected.
Is Elitone Covered By Insurance
In addition to determining the correct urinary incontinence ICD 10 code, treatment devices correlate with certain codes. HCPCS code E0740 applies to non-implantable pelvic floor muscle stimulators, including ELITONE. Note that PDAC recently reviewed this code and found that many previously covered devices, specifically those that provide biofeedback but do not provide e-stim, do not fall within the scope of E0740 and are not covered. To fall within the category of the code, the device must deliver stimulation that exercises the pelvic floor muscles.
ELITONE received approval to utilize E0740 shortly after it received FDA clearance. Many private insurers cover ELITONE and have published coverage decisions . Although requirements vary, most insurers have two stipulations: a prescription and failed improvement with four weeks of pelvic floor exercises.
Unlike other e-stim devices, ELITONE is also available as an FDA-cleared, over-the-counter product and can be purchased by patients directly from the ELITONE website. This is an excellent solution for patients without insurance coverage or who want immediate access to treatment.
Read Also: Why Do I Get Urinary Tract Infections Often
Gene Testing For Stress Urinary Incontinence
An UpToDate review on Evaluation of women with urinary incontinence states that The risk of urinary incontinence, particularly urgency incontinence, may be higher in patients with a family history. One study found that the risk of incontinence was increased for both daughters and sisters of women with incontinence. Twin studies attribute a 35 to 55 % genetic contribution to urgency incontinence/overactive bladder but only 1.5 % for stress incontinence.
Furthermore, an UpToDate review on Urinary incontinence in men does not mention genetic testing as a management option.
A Few Tips Before We Start:
1. You can supply 4 ICD-10 codes per 1500 claim form.
2. Some codes may require a 7th character. Be careful with these. If they require it but are less than 6 characters long, use an X as a placeholder in the additional spots. *The 7th character will indicate if the diagnosis is encountered as an initial encounter, subsequent encounter, or sequela of another issue.
3. Make sure that your documentation supports your coding choices.
4. To download your own free ICD-10 electronic index zip files:
a. go to Medicares ICD-10 webpage:
b. Click on CMS 2015 ICD-10-CM and GEMS on the left side of the screen
c. Download the 2015 Code Tables and Index
5. When looking up codes, dont just stop at the Index. The tabular section lists exclusions, code alsos, and other details that are critical.
Don’t Miss: Are Urinary Tract Infections Contagious
Transcutaneous Electrical Nerve Stimulation In The Treatment Of Overactive Bladder
In a randomized, double-blind, placebo-controlled study, Borch and associates evaluated the immediate effect on natural fill urodynamic parameters and bladder function during TENS in children with OAB and daytime UI . A total of 24 children with severe OAB and DUI underwent 48-hour natural fill urodynamics. After 24hours of baseline investigation, the children were randomized to either active continuous TENS or placebo TENS over the sacral S2-S3 outflow. The urodynamic recordings were analyzed manually for 3 different bladder contraction patterns resulting in a void. The number of bladder contractions not leading to a void was also calculated. Maximum voided volume and average voided volume were identified for both the baseline and the intervention day. It was found that TENS had no immediate objective effect on bladder capacity. The difference in MVV/EBC in the active TENS group=0.03±0.23 versus placebo TENS group=-0.01±0.10 . Furthermore, there was no significant difference in the proportion of different bladder contraction types between the 2 groups TENS did not significantly influence the number of bladder contractions not leading to a void. Results were presented as mean±SD. The authors concluded that there was no immediate objective effect of TENS on bladder activity assessed by natural fill urodynamics in children with OAB and DUI.
Bariatric Surgery For The Treatment Of Urinary Incontinence In Obese Women
In a meta-analysis, Zhang and colleagues examined the effectiveness of bariatric surgery in obese women with UI. Searches of PubMed, the Cochrane Library, and Embase databases were performed using “weight loss surgery/bariatric surgery/gastric bypass surgery” and “incontinentia urinae/uracratia/urinary incontinence/uroclepsia” in the title/abstract before January 2018. Then, meta-analysis was analyzed by Review Manager 5.3 . The SMD and OR were used to describe results of continuous variables and dichotomous variables, respectively. Pooled data showed that bariatric surgery reduced the incidence of UI in obese women at the follow-up of 6 months and 12 months and significantly reduced the BMI at 6 months and 12 months . In addition, bariatric surgery could also significantly increase the QOL and improve the function of pelvic floor disorders based on QOL questionnaires and Pelvic Floor Distress Inventory 20, respectively. The authors concluded that this meta-analysis demonstrated that bariatric surgery is an effective choice for obese women with UI however, more RCTs are needed to confirm these findings.
Furthermore, UpToDate reviews on Treatment of urinary incontinence in women and Treatment of urgency incontinence/overactive bladder in women do not mention bariatric surgery as a therapeutic option.
Read Also: Does Chemo Cause Urinary Incontinence
Other Experimental And Investigational Interventions For Urinary Incontinence
What Is The Severest Type Of Urinary Incontinence
Overactive bladder
Also known as urge or urgency incontinence, this condition causes the bladder muscles to contract and signal a need to urinate even if the bladder is empty. It causes an overwhelming urge to urinate immediately and may cause accidents if you dont make it to the restroom in time.
You May Like: Of A Urinary Tract Infection
Implantable Sacral Nerve Stimulators
Adjustable Retropubic Suburethral Sling For Stress Urinary Incontinence
In a single-center, prospective study, Leizour and associates evaluated the safety and effectiveness of the adjustable suburethral sling Remeex in the treatment of male SUI. Participants were patients treated for SUI after radical prostatectomy or transurethral resection of prostate. The severity of incontinence was evaluated by the number of pads used per day. Success rate, complications and number of adjustments were studied. From February 2011 to May 2015, Remeex was implanted in 25 patients. The average pre-operative number of pads used per day was 3.8 . Sling tension has been adjusted the day after surgery in all patients. Mean follow-up was 31 months . During follow-up, 6 patients did not need any re-adjustment and 15 patients had to be re-adjusted. One Remeex system had to be completely removed because of a sub-occlusive syndrome 3 patients had early infection requiring partial system removal . At the end of follow-up, 9 patients were cured , 9 patients were significantly improved and 7 patients were not improved 5 patients were waiting for a new re-adjustment. The authors concluded that in this short series of patients who had prostatic surgery, at mid-term follow-up, the placement of an adjustable suburethral sling was associated with an improvement or cure of UI symptoms in 2/3 of cases.
Read Also: Does Cranberry Juice Help Prevent Urinary Tract Infections
Test Stimulation Of The Interstim
The InterStim product labeling states that, in clinical studies, subjects underwent anywhere from 1 to 6 test stimulation procedures before implantation of InterStim.
The Medtronic InterStim test stimulation lead kit manual stated that Of the 260 patients who qualified for implantation, 169 had a successful result during their first test stimulation procedure. Of the remaining 91 patients, 56 obtained a successful result during a second test stimulation, and 35 obtained a successful result during three or more test stimulations. Reasons for repeat test stimulation procedures included inadequate responses to test stimulation or technical problems . The safety and effectiveness of this therapy has not been established for pediatric use , patients with neurological disease origins, such as multiple sclerosis or diabetes, and bilateral stimulation.
Other Urinary Incontinence Interventions
Pelvic Muscle Trainers
Note: Aetna does not cover the Athena pelvic muscle trainer, Gyneflex, Kegelmaster, Leva Pelvic Floor Trainer, or similar devices for the treatment of UI because these devices are considered exercise machines, and they do not meet Aetna’s definition of covered durable medical equipment . Most Aetna plans exclude coverage of exercise devices. Please check benefit plan descriptions for details. In addition, such exercise devices do not meet Aetna’s definition of covered DME because they are not primarily medical in nature and/or are normally of use to persons who do not have an illness or injury.
Recommended Reading: Leg Pain And Urinary Incontinence
Magnetically Controlled Endourethral Artificial Urinary Sphincter
Mazzocchi and colleagues stated that UI is a widespread dysfunction that affects more than 300 million people worldwide. At present, no technological solutions are able to restore continence in a minimally invasive and effective way. These researchers described the design, fabrication, and testing of a novel artificial endourethral urinary sphincter that attempts to fully restore continence. The device can be inserted/retracted in a minimally invasive fashion without hospital admission, does not alter the body scheme and can be applied to both women and men. The device core is a uni-directional polymeric valve and a magnetically activated system, which is able to modulate its opening pressure. Bench tests and ex-vivo tests on a human cadaver demonstrated that the device was able to fully restore continence and allowed urination when desired. The authors concluded that the proposed system showed a high potential as a technological solution that may restore a normal daily life in patients affected by UI. These preliminary findings need to be validated by well-designed studies.
Other Disorders Of Urinary System
- 20162017201820192020202120222023Non-Billable/Non-Specific Code
- Female stress incontinence
- Female urinary stress incontinence
- Male urinary stress incontinence
- Urinary stress incontinence, male
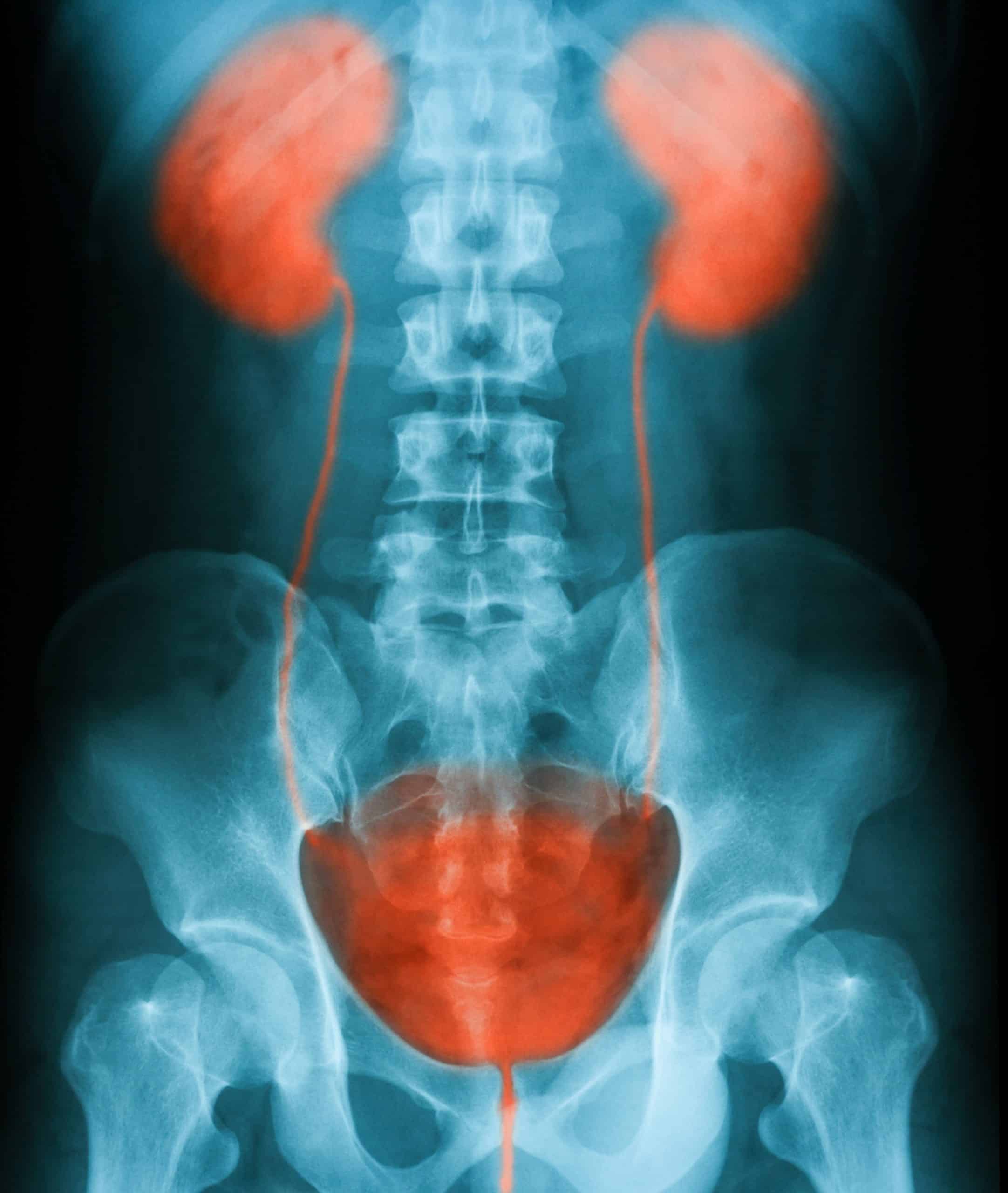
- Involuntary discharge of urine as a result of physical activities that increase abdominal pressure on the urinary bladder without detrusor contraction or overdistended bladder. The subtypes are classified by the degree of leakage, descent and opening of the bladder neck and urethra without bladder contraction, and sphincter deficiency.
- Loss of less than 50 ml of urine occurring with increased abdominal pressure
- Loss of urine occurring with increased abdominal pressure
- Loss of urine occurring with increased abdominal pressure.
- 695 Kidney and urinary tract signs and symptoms with mcc
- 696 Kidney and urinary tract signs and symptoms without mcc
- 742 Uterine and adnexa procedures for non-malignancy with cc/mcc
- 743 Uterine and adnexa procedures for non-malignancy without cc/mcc
- 760 Menstrual and other female reproductive system disorders with cc/mcc
- 761 Menstrual and other female reproductive system disorders without cc/mcc
You May Like: Can A Urinary Tract Infection Cause Diarrhea
Did I Prescribe The Right Treatment
When youve diagnosed the patient and figured out the correct urinary incontinence ICD 10 code, its time to recommend an appropriate treatment. Primary care physicians and gynecologists may not be familiar with all the at-home options to treat their stress urinary incontinence patients. Typical suggestions include Kegel exercises and limiting fluid intake, and currently, there are no medications approved to treat stress urinary incontinence. Invasive treatments include surgery, internal tissue manipulation, and intravaginal monitoring and stimulation, plus these treatments typically require a specialists care.
For patients with mild to moderate incontinence symptoms, it may be preferential for the primary care physician or gynecologist to provide conservative care directly. This approach results in more immediate care for the patient, continuity of care to monitor progress, and minimized costs.
- Want to supplement or have limited access to pelvic floor physical therapy.
- Have trouble performing Kegel exercises correctly .
- Prefer the convenience and privacy of in-home treatment.
- Need care after their 6-week postpartum checkup.
Starting To Worry About How To Apply Icd
Im here to walk you through some examples of typical patient codes. Remember, this coding system is not as cookie-cutter as ICD-9 was, and its brand new to all of us. So, we cannot guarantee that all payors will reimburse specific codes. While there may be some easy crosswalks, not all codes will be simple. I encourage you to share your success and unsuccessful stories among your colleagues so that we can all learn together.
Read Also: Urinary Tract Infection During Pregnancy
Determinants Of Referrals Analysis
The cohort for identifying determinants of referrals was derived from the CPRD data set and comprised women aged 18 years who had an index diagnosis of UI between 1 April 2004 and 31 March 2014. An index diagnosis of UI was defined among women who had no earlier record of a UI symptom/diagnosis or treatment within the 12 months prior to the date of first diagnosis in the study period. For the referral analyses, women were followed up until the date of the GP visit that they were referred to a UI specialist, transfer out of practice, death or to 1 April 2014. Women with < 12 months of UTS data prior to index diagnosis were excluded. Women were also excluded if the follow-up period was < 30 days.
Pelvic Floor Electrical Stimulation
You May Like: Male Urinary Tract Infection Signs And Symptoms