Control Your Urge To Urinate
You may be able to control, or suppress, the strong urge to urinate, which is called urge or urgency suppression. With this type of bladder training, you can worry less about finding a bathroom in a hurry. Some people distract themselves to take their minds off needing to urinate. Other people find that long, relaxing breaths or holding still can help. Doing pelvic floor exercises to strengthen your pelvic floor also can help control the urge to urinate. Quick, strong squeezes of the pelvic floor muscles can help suppress urgency when it occurs, which may help you get to the toilet before you leak.
Current Therapies For Stress Urinary Incontinence
There are a variety of therapies for SUI, including conservative measures involving physical therapy , bladder retraining, anti-incontinence devices , and a combination of these strategies. These conservative therapies often fail or are unsatisfactory options for patients with more severe SUI. Periurethral bulking agents, retropubic suspension procedures, and various transvaginal anti-incontinence procedures are more invasive options.
The one type of treatment of SUI that has been sufficiently devoid of novel strategies is pharmacologic therapies that increase urethral resistance. Although several medications have been used to treat SUI, none is FDA-approved and none is very successful. Once patients have completed a full evaluation, initial treatment often consists of behavioral modification, followed by surgical therapies. The concept of pharmacologic therapy as a first-line therapy for SUI is presented in this paper, along with the possibility of synergy between pharmacologic therapy and current conservative measures to help improve our current treatment strategies for SUI.
Transvaginal Needle Suspension Procedures
Transvaginal needle suspension techniques evolved as a minimally invasive alternative to the retropubic procedures for SUI due to urethral hypermobility. The original transvaginal needle suspension was first described by Armand Pereyra, MD, in 1959. Since then, however, many modifications of this procedure have been reported. The common feature of each of these modifications is that the anterior abdominal wall fascia is not incised and the suspending sutures are passed through the retropubic space from the vagina to the anterior abdominal wall with a specialized long ligature passer.
Advantages to the transvaginal approach include the avoidance of a large, transfascial abdominal incision shorter operative times less postoperative discomfort shorter hospital stay and the ability to repair coexisting vaginal pathology through the same or slightly extended incision. Disadvantages include a potentially lower long-term cure rate poor intraoperative visualization risk of injury to the bladder and urethra during blind passage of the needles through the retropubic space risk of significant bleeding in the retropubic space with poor operative access from the vaginal incisions and, lastly, infection or erosion of a foreign body if suture buttresses are utilized .
Recommended Reading: How Treat Urinary Tract Infection Naturally
Basic Evaluation Of Stress Urinary Incontinence
When women are evaluated for SUI, counseling about treatment should begin with conservative options. The minimum evaluation before primary midurethral sling surgery in women with symptoms of SUI includes the following six steps: 1) history, 2) urinalysis, 3) physical examination, 4) demonstration of stress incontinence, 5) assessment of urethral mobility, and 6) measurement of postvoid residual urine volume.
Targeting Both The 1 Receptors And The 5
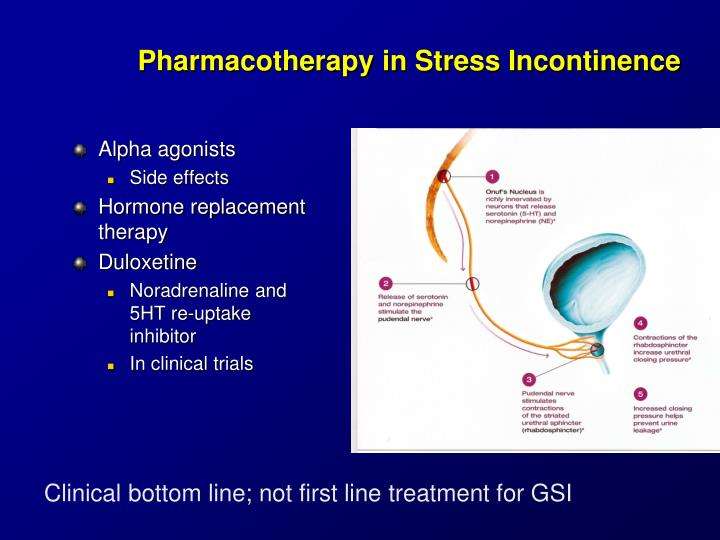
There are several possible methods of increasing the effects of serotonin and norepinephrine on the storage mechanisms of the lower urinary tract. One method is to block the reuptake of these neurotransmitters at the nerve terminals, thereby increasing receptor stimulation . Duloxetine and venlafaxine are two such drugs that block both serotonin and norepinephrine reuptake.
Monoaminergic synapse, illustrating monoamine reuptake from the synaptic cleft and monamine reuptake inhibition.
Read Also: Urinary Tract Infection What Is It
Review Of Urethral Continence Mechanisms
The sympathetic, parasympathetic, and somatic nervous systems all contribute to urethral innervation coordinated by the central nervous system. These neural pathways control the function of the bladder and urethra to maintain continence. A simple diagram of the involved neuropathways is shown in Figure 1.
Sympathetic and parasympathetic control of urethral smooth muscle. Red and green arrows indicate inhibition and excitation, respectively.
Strengthening The Pelvic Floor Muscles
It is important that you exercise the correct muscles. Your doctor may refer you to a continence advisor or physiotherapist for advice on the exercises. They may ask you to do a pelvic floor exercise while they examine you internally, to make sure you are doing them correctly. The sort of exercises are as follows:
Learning to exercise the correct muscles
- Sit in a chair with your knees slightly apart. Imagine you are trying to stop wind escaping from your back passage . You will have to squeeze the muscle just above the entrance to the anus. You should feel some movement in the muscle. Don’t move your buttocks or legs.
- Now imagine you are passing urine and are trying to stop the stream. You will find yourself using slightly different parts of the pelvic floor muscles to the first exercise . These are the ones to strengthen.
- If you are not sure that you are exercising the right muscles, put a couple of fingers into your vagina. You should feel a gentle squeeze when doing the exercise. Another way to check that you are doing the exercises correctly is to use a mirror. The area between your vagina and your anus will move away from the mirror when you squeeze.
- The first few times you try these exercises, you may find it easier to do them lying down.
Recommended Reading: What Is The Antibiotic For Urinary Tract Infection
Some General Lifestyle Measures Which May Help
- Your GP may refer you to the local continence adviser. Continence advisors can give advice on treatments, especially pelvic floor exercises. If incontinence remains a problem, they can also give lots of advice on how to cope. Examples include the supply of various appliances and aids such as incontinence pads, etc.
- Getting to the toilet. Make this as easy as possible. If you have difficulty getting about, consider special adaptations like a handrail or a raised seat in your toilet. Sometimes a commode in the bedroom makes life much easier.
- Obesity. Stress incontinence is more common in women who are obese. Weight loss is advised in those who are overweight or obese. It has been shown that losing a modest amount of weight can improve urinary incontinence in overweight and obese women. Even just 5-10% weight loss can help symptoms.
- Smoking can cause cough which can aggravate symptoms of incontinence. It would help not to smoke.
Can Incontinence Be Prevented
Different events throughout your life can lead to many of the things that cause incontinence. The muscles that support your pelvic organs can weaken over time. For women, these muscles can also be weakened by big life events like pregnancy and childbirth. However, in the same way you work out to build strength in your legs or arms, you can do exercises to strengthen your pelvic floor muscles. Doing exercises to strengthen your pelvic muscles may not prevent you from having any issues with incontinence, but it can help you regain control of your bladder. Maintaining a healthy body weight can also help with bladder control. Talk to your healthcare provider about the best ways to maintain strong pelvic floor muscles throughout your life.
Don’t Miss: Clearing Urinary Tract Infection Naturally
Urinary Incontinence In Older Adults
Urinary incontinence means a person leaks urine by accident. While it may happen to anyone, urinary incontinence is more common in older people, especially women. Incontinence can often be cured or controlled. Talk to your healthcare provider about what you can do.
What happens in the body to cause bladder control problems? The body stores urine in the bladder. During urination, muscles in the bladder tighten to move urine into a tube called the urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder dont work the way they should, urine can leak. Incontinence typically occurs if the muscles relax without warning.
What Are The Types Of Urinary Incontinence
More than half of people with stress incontinence also have urge incontinence. Having both stress and urge incontinence is known as mixed incontinence. An overactive bladder causes urge incontinence. This type of urinary incontinence causes you to leak urine when you feel an urgent need to pee.
Overflow incontinence is a different type of urinary incontinence. It causes you to leak urine because your bladder is too full or you cant completely empty it.
You May Like: Is Azithromycin Good For Urinary Tract Infection
Causes Of Urinary Incontinence
Incontinence can happen for many reasons. For example, urinary tract infections, vaginal infection or irritation, constipation. Some medicines can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
- Weak bladder muscles
- Overactive bladder muscles
- Weak pelvic floor muscles
- Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinsons disease
- Blockage from an enlarged prostate in men
- Diseases such as arthritis that may make it difficult to get to the bathroom in time
- Pelvic organ prolapse, which is when pelvic organs shift out of their normal place into the vagina. When pelvic organs are out of place, the bladder and urethra are not able to work normally, which may cause urine to leak.
Most incontinence in men is related to the prostate gland. Male incontinence may be caused by:
- Prostatitisa painful inflammation of the prostate gland
- Injury, or damage to nerves or muscles from surgery
- An enlarged prostate gland, which can lead to Benign Prostate Hyperplasia , a condition where the prostate grows as men age.
What Is Urinary Incontinence

Many people experience involuntary leakage of urine from the bladder. This condition is called urinary incontinence. It affects nearly a quarter to a third of men and women in the United States. That is millions of Americans.
Urinary incontinence is the leaking of urine from the bladder that you cant control. There are different kinds of urinary incontinence, and not all types are permanent. An experienced doctor can help you find the best treatment for your urinary incontinence.
Stress urinary incontinence is when the muscles arent strong enough to hold urine in the body. SUI shows itself through physical symptoms, including involuntary leaking of urine through the bladder when active.
Overactive bladder is a strong sudden urge to urinate, which may or may not cause urine to leak from the bladder.
In some cases, people experience a combination of both SUI and OAB. This shows itself through physical symptoms. If this is the case for you, you will find involuntary leaking of urine through the bladder and strong sudden urges to urinate that you cant control.
Overflow incontinence is when the bladder isnt able to empty itself completely. Overflow incontinence shows itself through physical symptoms, including constant dribbling of small amounts of urine when the bladder is full.
These symptoms are not just physical. Urinary incontinence has emotional and psychological effects, too.
Read Also: Treat Urinary Tract Infection Over The Counter
Assessment Of Urethral Mobility
Anti-incontinence surgery is more successful in women with urethral mobility, defined as a 30 degree or greater displacement from the horizontal when the patient is in a supine lithotomy position and straining. The presence of urethral mobility indicates uncomplicated SUI. Lack of urethral mobility is associated with a 1.9-fold increase in the failure rate of midurethral sling treatment of SUI 13. The cotton swab test has been the traditional assessment of urethral mobility 14, but other methods of evaluating urethral mobility include measurement of point Aa of the POP Quantification system, visualization, palpation, and ultrasonography 151617. Patients who lack urethral mobility may be better candidates for urethral bulking agents rather than sling or retropubic anti-incontinence procedures.
Medical Treatments For Stress Urinary Incontinence
If you are living with bladder leaks, you should know that medical treatments for stress urinary incontinence are available that may bring much needed relief.
At Pelvital, weve introduced Flyte, a non-surgical, use-at-home option that strengthens the pelvic floor muscles to treat SUI. As a first-line treatment, Flyte will help many women to treat at home and avoid more expensive or inconvenient medical treatments for stress urinary incontinence.
According to the Office on Womens Health, U.S. Department of Health and Human Services, its a good idea to talk to your doctor about other medical treatments if you arent able improve bladder leaks with home-based measures. Medical treatments include:
Medicine. After menopause, applying vaginal creams, rings, or patches with estrogen can help strengthen the muscles and tissues in the urethra and vaginal areas. A stronger urethra will help with bladder control. Learn more about menopause treatments on the womenshealth.gov site.
Bulking agents. Your doctor can inject a bulking agent, such as collagen, into tissues around the bladder and urethra to cause them to thicken. This helps keep the bladder opening closed and reduces the amount of urine that can leak out.
Surgery. Surgery for urinary incontinence is not recommended if you plan to get pregnant in the future. Pregnancy and childbirth can cause leakage to happen again. The two most common types of surgery for urinary incontinence are :
Also Check: What Vitamins Are Good For Urinary Tract Infections
Who Suffers From Stress Incontinence
According to the National Institute of Diabetes and Digestive and Kidney Diseases , women are twice as likely as men to suffer from involuntary leakage. The most common causes of stress incontinence among women are pregnancy and childbirth, especially having multiple vaginal deliveries. During pregnancy and childbirth, the sphincter and pelvic muscles stretch out and are weakened.
Older age and conditions that cause a chronic cough can also cause stress incontinence. This condition can also be a side effect of pelvic surgery.
Some women only suffer from stress incontinence during the week before they get their period. The NIDDK explains that estrogen drops during this phase of the menstrual cycle, which can weaken the urethra. This is not common though.
Among men, prostate surgery is a common cause of stress incontinence. The prostate gland surrounds the male urethra, and its removal can result in the loss of support of the urethra.
Other risk factors for stress incontinence include:
- smoking due to chronic cough
- any other condition associated with chronic cough
- excessive caffeine and alcohol use
- obesity
Treatment for stress incontinence varies according to the underlying cause of your problem. Your doctor will help you come up with a treatment plan using a combination of medications and lifestyle adjustments.
Pelvic Floor Muscle Exercises
The pelvic floor is layers of muscles that stretch from the pubic bone to the coccyx and then from side-to-side. These muscles help to support the bladder and bowel plus the womb in women. These muscles can become weak through trauma such as childbirth or surgery, changing hormones, persistent coughing or chronic constipation. When these muscles become slack it can weaken the opening to the bladder causing urine to leak out when placed under pressure. These exercises can help to strengthen the pelvic floor and reduce the occurrence of leaking. Click to read about pelvic floor muscle exercises.
Read Also: How To Get Rid Of A Urinary Tract Infection
Surgical Treatment Of Female Stress Urinary Incontinence : Aua/sufu Guideline
To cite this guideline:Kobashi KC, Albo ME, Dmochowski RR et al: Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J Urol 2017 198: 875.
AUA/SUFU Guideline: Published 2017
Stress urinary incontinence is a common problem in the field of Female Urology. This guideline evaluates both the index patient, defined as an otherwise healthy female considering surgical therapy for the correction of SUI, as well as the non-index patient, which includes those with high-grade prolapse as well as geriatric patients. Topics covered include evaluation and patient counseling, minimally invasive surgery procedures, outcomes assessment, and overall bladder health.
Presentation from the 2017 Annual Meeting Español translated guideline courtesy of Confederacion Americana de Urologia
Citation: Kobashi KC, Albo ME, Dmochowski RR et al: Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J Urol 2017 198: 875.
Treatment Of Nocturnal Enuresis
While nocturnal enuresisdefined as involuntary loss of urine during sleep that occurs at least twice a week in children older than 5 years of age for at least 3 monthsis the most common urologic complaint in pediatric patients, it also affects a significant number of adults. Nocturnal enuresis in adults may have multiple underlying pathologies, and treatment should first target identifiable etiologies, although a generalized approach can then be followed, utilizing behavioral and lifestyle modifications followed by medical therapy.
Such basic measures as evening fluid restriction and daytime bladder training can be beneficial. Desmopressin decreases nighttime urine production it is administered orally for primary nocturnal enuresis and intranasally or sublingually for nocturnal polyuria. Imipramine has been one of the most common pharmacologic therapies. Oxybutynin and other anticholinergics have been used.
Although pharmacologic treatment can help, the underlying disorder often returns after discontinuation. Conditioning therapy with moisture-sensitive alarms are effective. Positive results usually persist even after the device is removed.
Don’t Miss: How Long Does Urinary Retention Last After Botox
Extracorporeal Magnetic Resonance Therapy
Extracorporeal magnetic resonance therapy has been introduced as a therapy for stress incontinence. The NeoControl unit was approved by the Food and Drug Administration for this purpose in 2000. Resonating magnetic flux within a magnetic field induces electrical depolarization of targeted nerves and muscles. No probes are required. The patient simply sits on a chair containing the magnetic device.
A small study achieved an improvement rate of 77% after 8 weeks of therapy, with 56% of patients being completely dry. However, a 3-year follow-up study found that the benefits tend to be temporary: at 6 months, the recurrence rate was 53%.
Pelvic Floor Muscle Training

Pelvic floor muscle training can be one of the most important components of behavioral therapy. PFMT exercises help the patient strengthen the muscles of the pelvic floor. Since Arnold Kegel, MD, first described these exercises almost 50 years ago, numerous studies have evaluated the efficacy and durability of PFMT, with conflicting results.
The levator ani muscle group and the surrounding fascia comprise the pelvic floor and provide the supportive mechanism for the pelvic organs. This group of muscles is found at the base of the pelvic floor and is composed of approximately 70% slow-twitch and 30% fast-twitch muscle fibers. Slow-twitch muscle fibers produce less force on contraction and assist in improving muscle endurance by generating a slower, more sustained, but less intense contraction. Fast-twitch muscle fibers, which aid in quick and forceful contractions, can be used during sudden increases of intraabdominal pressure by contributing to urethral closure. PFMT exercises consist of repeated, high-intensity, pelvic muscle contractions of both types of muscle fibers.
A recent study by Diokno and colleagues was the first to demonstrate that a structured behavioral modification and PFMT program may actually prevent the subsequent development of urinary incontinence in older women. This study has important clinical and public health implications. Further work to substantiate these findings is anticipated.
Read Also: Best Probiotic For Urinary Tract Infection