Pathophysiological Consequences Of Spinal Cord Disease For Bladder Function
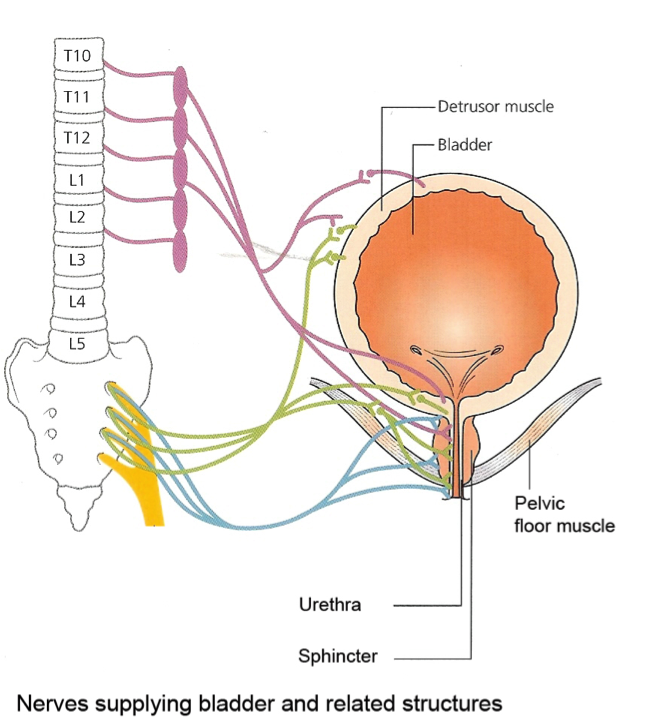
Trans-spinal pathways connect the pontine micturition centres to the sacral cord and intact connections are necessary to effect the reciprocal activity of the detrusor and sphincter needed to `switch’ between storage and voiding. Following disconnection from the pons this synergistic activity is lost and the result is that the sphincter tends to contract when the detrusor is contracting, a condition known as `detrusor-sphincter dyssynergia’. In addition new reflexes emerge to drive bladder emptying and cause detrusor hyperreflexia. Immediately following spinal cord transection and during the phase of spinal shock, the bladder is acontractile but gradually over the course of some weeks, reflex detrusor contractions develop in response to low volumes of filling. The neurophysiology of this recovery has been studied in the cat and it has been proposed that following spinal injury and damage to the pontine micturition centre, C fibres emerge as the major afferents forming a spinal segmental reflex which results in automatic voiding . It is assumed that the same pathophysiology occurs in man and the response to intravesical capsaicin of patients following acute traumatic spinal cord injury or the chronically progressive spinal cord disease multiple sclerosis suggests this may be the case .
Complications Of Neurological Bladder Problems
Neurological disorders of the urinary tract can cause a variety of long term complications the most serious of which is kidney damage resulting in renal failure. Early diagnosis and management of neurological urinary tract problems can prevent irreversible deterioration in the function of the kidneys as well as bladder and urinary sphincter.
Potential complications from neurological urinary tract problems include:
- Reduced quality of life
Bladder Dysfunction And Valve Bladder Syndrome
Consequent to exposure to obstruction from its earliest development, the bladder is necessarily the focus of management and rehabilitation throughout the life of a boy diagnosed with PUVs .The extent of remodeling and subsequent functional compromise may vary, but the bladder and its dysfunction begins a cascade of pathophysiologic changes including voiding dysfunction, urinary reflux, and worsening of renal dysplasia and obstructive uropathy. The ultimate manifestation of this dysfunction is the valve bladder syndrome.
Urodynamics plays an important role in monitoring an affected child’s progression through various well-described changes in bladder function throughout childhood.The bladder evolves through three distinct contractility patterns throughout childhood: detrusor hyperreflexia in infancy and early childhood decreasing intravesical pressures and improved compliance bladder in childhood and increased capacity bladder with hypocontractility and atony in adolescence . Holmdahl etal. stressed that the pattern outlined here overlaps in most children, emphasizing that the patterns described earlier are not arbitrary or destined to happen, but rather useful guideposts in monitoring and helpful in offering management solutions and assessing the effectiveness of intervention over the long-term .
In , 2011
Recommended Reading: Treat Urinary Tract Infection Over The Counter
What Makes Yale Medicine’s Approach To Neurogenic Bladder Unique
Patients can expect the most advanced treatment options available for neurogenic bladder, including sacral neuromodulation bladder injections and complex bladder reconstructive surgery.
Our goal is to provide a patient-centered approach,” says Dr. Chai. “So we work with your medical doctors including primary care physicians, neurologists, and specialists in physical medicine and rehabilitation to ensure that you are taken care of holistically.
Case 1 Benign Rolandic Epilepsy
An 8-year-old female presented with persistent bedwetting and occasional daytime incontinence. Her past medical history was notable only for vesicoureteral reflux, chronic otitis media with tympanostomy, and constipation. Because she would wait âuntil the last minuteâ to urinate, behavioral measures first implemented included fluid restriction before bedtime. Trials of antibiotics and antispasmodics were discontinued after a voiding cystouretherogram showed an insignificant amount of reflux. Past physical examination by the family doctor showed normal external genitalia and positive anal reflex with good tone, and unremarkable neurological examination.
At age 8, to the persistence of her urinary issues, she was started on imipramine, without benefit. Around that time she presented to our clinic following a brief episode of right sided facial twitching during sleep with deviation of the mouth to the right. The mother, who witnessed the episode, reported 30-seconds duration and no incontinence. When asked regarding occurrence of similar symptoms, the patient recounted an episode six months prior when after a bath she had similar lip twitching that lasted for 10 to 15 seconds. There were no headaches, bowel or bladder incontinence during or following the episode and no personal or family history of seizures. EEG showed multifocal epileptiform discharges more prominent in the fronto-parietal area, consistent with BRE.
You May Like: What Are The Symptoms Of A Severe Urinary Tract Infection
Who Is At Risk For Urinary Incontinence
In adults, you are at higher risk of developing UI if you:
- Are female, especially after going through pregnancy, childbirth, and/or menopause
- Are older. As you age, your urinary tract muscles weaken, making it harder to hold in urine.
- Are a man with prostate problems
- Have certain health problems, such as diabetes, obesity, or long-lasting constipation
- Are a smoker
- Have a birth defect that affects the structure of your urinary tract
In children, bedwetting is more common in younger children, boys, and those whose parents wet the bed when they were children.
I Have A Neurological Problem
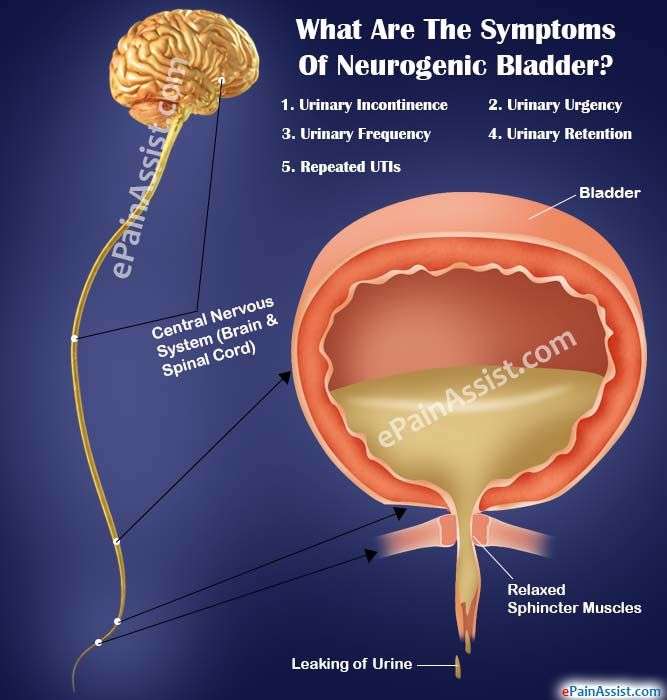
Neurological conditions can affect the parts of the bodys nervous system that regulate urine storage and control when you pass urine .
For that reason, urinary incontinence is particularly common in people with conditions such as multiple sclerosis, spinal cord injury, diabetes and Parkinsons disease. Urinary incontinence can also develop after an infection of the brain, heavy metal poisoning or major pelvic surgery.
In particular, neurological problems can lead to:
- Urge incontinence
- Stress incontinence
- Difficulties in emptying the bladder
In general, neurogenic bladder is an umbrella term which is often used to refer to any urinary incontinence symptom that is associated with a neurological condition. Of course, the exact symptoms will differ from person to person, which is why it is important to discuss your situation with a healthcare professional. Find out more about the different types of incontinence here.Many treatments are effective at treating urinary incontinence in people with neurological problems. These include:
- Lifestyle changes and behavioural treatments . These include simple dietary changes, bladder training, and the keeping of a bladder diary.
- Mechanical treatments such as catheters .
- Bladder relaxants .
- Bladder injections .
- Surgical interventions and sacral neuromodulation .
If you believe that your urinary incontinence is related to a neurological condition, you might find the following tips useful:
Video diary before bladder injections:
References
Read Also: What Cause Urinary Tract Infection In Male
Bladder And Bowel Dysfunction
BBD is an umbrella term that includes lower urinary tract dysfunction and bowel dysfunction .Patients with BBD experience a spectrum of symptoms and require a thorough history to guide therapy. The history should be obtained from the caretaker as well as the child because their perceptions may differ.
Patients with BBD may have storage and voiding symptoms. Storage symptoms include urinary frequency, urgency, and nocturia as well as urinary incontinence. The examiner should further assess incontinence as continuous versus intermittent. Intermittent incontinence should be further categorized as daytime incontinence and enuresis . Voiding symptoms include hesitancy, straining, weak stream, intermittency, and dysuria. Other behaviors such as holding maneuvers, the sensation of incomplete emptying, and pain should be assessed. The examiner should also specifically inquire about the course of toilet training, whether there was an asymptomatic period, and whether there is any history of UTIs. The close relationship between bladder and bowel function requires screening of bowel dysfunction, preferably with a bowel diary using the Bristol Stool Form Scale . Finally, the examiner must differentiate patients whose symptoms are due to other underlying causes. For example, continuous leakage may suggest an ectopic ureter. Symptoms consistent with detrusor sphincter dyssynergia may be due to occult spinal dysraphism. Urinary retention may be caused by posterior urethral valves.
Bladder Dysfunction And Brainstem Lesions
In 1926 Holman noted that voiding difficulty could be a sign of posterior fossa tumours and in the series of patients with brain tumours voiding difficulty was reported to occur in 46 out of 152 patients with posterior fossa tumours while urinary incontinence occurred in only 3 . Renier and Gabreels found urinary retention in 12 out of 17 children with pontine glioma. There have also been a number of case histories of patients presenting with difficulty with micturition and various brainstem pathologies .
Read Also: Natural Remedies For Male Urinary Tract Infection
How Is Urethral Incontinence Treated
Treatment is based on your pet’s specific diagnosis. Medications that increase urethral sphincter tone such as phenylpropanolamine or imipramine, or hormone replacements such as estrogen or diethylstilbestrol are commonly used alone and in combination. Many dogs that respond poorly to PPA alone will benefit from a combination of PPA and DES. Approximately 70% of all cases respond well to medical therapy alone. GnRH analogs may be considered in severe or refractory cases. With long-term usage, the patient’s blood and urine should be periodically tested to ensure that there are no untoward side effects. Your veterinarian will prescribe the best treatment for your pet’s individual needs.
“Treatment is based on your pets specific diagnosis.”
New research has focused on collagen injections to improve urethral closure. This surgical solution holds promise and should be discussed with your veterinarian to determine if any of the surgical specialists in your area are performing this procedure.
Incomplete Bladder Emptying Or Urinary Retention
Incomplete emptying can exacerbate detrusor hyperreflexia, and an overactive bladder constantly stimulated by a residual volume will respond by contracting and producing symptoms of urgency and frequency. Incomplete emptying is particularly likely to occur in patients with spinal cord disease due to a combination of detrusor sphincter dyssynergia occurring during attempts to void and poorly sustained detrusor contractions during the voiding phase.
Since there is no medication which causes effective detrusor contraction at a convenient moment the best option to deal with incomplete emptying or retention has been to use intermittent catheterization. Sterile intermittent catheterization was first introduced in the 1960s , but it was then found that a clean rather than sterile technique was adequate . Performed for children with spina bifida and the elderly with disorders of complete bladder emptying it has proved highly effective in many patients with multiple sclerosis and various other bladder disorders characterized by incomplete emptying.
Read Also: Can An Iud Cause Urinary Tract Infections
Spine Disorders With Potential To Cause Nbd
- is a common cause of neurogenic bladder dysfunction. The spinal cord need not be severed to cause paralysis below the injured level of the spine . Bruising of the spinal cord or inadequate blood flow can damage the cord’s ability to transmit nerve signals.
- occurs when the spinal nerve roots in the lower back are compressed. Although cauda equina syndrome is a rare occurrence, it is a serious medical situation requiring urgent care.
Causes of CES include:
What Is Neurogenic Bladder
Neurogenic bladder is when a problem in your brain, spinal cord, or central nervous system makes you lose control of your bladder. You may pee too much or too little. You could have symptoms of both overactive bladder and underactive bladder . You may not be able to fully empty it.
Itâs normal to have some stress and anxiety if you canât control when you urinate. Talk to your doctor about whatâs going on as soon as possible so you can start on a treatment to help manage your symptoms.
Don’t Miss: Tea Tree Oil Urinary Tract Infection
In This Video Dmx Displays Prolotherapy Before And After Treatments
- In this video, we are using a Digital Motion X-Ray to illustrate a complete resolution of a pinched nerve in the neck and accompanying symptoms of cervical radiculopathy.
- A before digital motion x-ray at 0:11
- At 0:18 the DMX reveals a completely closed neural foramina and a partially closed neural foramina
- At 0:34 DXM three months later after this patient had received two Prolotherapy treatments
- At 0:46 the previously completely closed neural foramina is now opening more, releasing pressure on the nerve
- At 1:00 another DMX two months later and after this patient had received four Prolotherapy treatments
- At 1:14 the previously completely closed neural foramina is now opening normally during motion
Urinary Incontinence Related To A Neurological Condition
Urinary incontinence is the leakage of urine when you do not mean to urinate . It is a common condition with many causes and is particularly common in people with neurological conditions.
Neurological conditions affect the body’s nervous system, involving damage to the brain, spinal cord or other nerves. The nervous system plays an important role in regulating the storage of urine in the bladder and coordinating and controlling when you pass urine. Damage to the nervous system may cause problems that affect the lower urinary tract. The lower urinary tract is the lower part of the urinary system, which includes the bladder, the tube that takes urine from the bladder and the muscles that control the release of urine . People with neurological conditions may have problems with the bladder or the sphincters or both, including:
-
Problems with bladder storage, for example, needing to urinate urgently and/or frequently, or incontinence. One type is urge incontinence, when you feel a sudden need to urinate and then can’t stop some urine leaking out. This is often caused by the bladder muscle contracting before the bladder is full .
-
Stress incontinence, which involves leakage of urine when you strain, for example, on coughing or sneezing, or with the effort of lifting a heavy object.
-
Problems with bladder emptying, such as having a delay between trying and starting to urinate, a slow or weak urinary stream, the need to strain or problems with urine being held in the bladder.
You May Like: Urinary Tract Infection And Alcohol
Neurogenic Bladder Control Symptoms & Treatment
Neurogenic bladder is a nervous system condition that keeps you from having normal bladder control. It happens when the nerves that control your bladder get damaged, often due to illness or injury.There are two types of neurogenic bladder.
- Overactive bladder causes you to have little or no control over your urination. It can also cause you to feel a sudden or frequent need to urinate. .
- Underactive bladder occurs when your bladder muscles lose their ability to hold your urine. Youre no longer able to sense when your bladder is full or to empty it completely, so it over-fills and urine leaks out. .
There Is A Connection Between Urinary Problems And Cervical Neck Pain The Vagus Nerve And Blood Pressure
The Vagus Nerve controls the muscle movement of the bladder during urination. If you look at the illustration above you will see where the Vagus nerve is closely related to the C1 C2 C3 vertebrae. While doctors usually discuss the vagus nerve in singular sense, there are two vagus nerves, one on each side of the neck and in combination they are referred to as the vagal nerves. This means that the degenerative damage in your neck can significantly impact the function of one or both vagus nerves.
There has been some degree of controversy as to whether or not the vagus nerves do provide nerve impulses and function to the bladder. It should not be far fetched to think they do. The vagus helps regulate your heartbeat, the vagus helps regulate your breathing, your vagus regulates functions of your digestive tract. Wouldnt it be within the realm of possibility that the vagus could also regulate the bladder? Lets get to the science so we may be able to explain how treating your neck pain can, among other things, help regulate your bladder.
We are going to go back to a 1987 study performed on dogs, that makes a connection to neck area pain, the heart, and urinary bladder problems. If your neck pain includes problems of regulating heartbeat, you may find a long-sought answer to some of your problems.
Here are the highlights:
What did the researchers find?
What does this mean to you?
Urinary problems, heart rate, blood pressure, seemingly all have a common neck component.
Don’t Miss: Does Cranberry Juice Clean Urinary Tract
Urinary Incontinence And The Bladder
Spinal disorders or injuries that cause nerve compression or damage may cause Neurogenic Bladder Disorder also termed Bladder Dysfunction. NBD means the patient has problems with urination. The term neurogenic refers to the nerve tissues that supply and stimulate an organ or muscle to function properly. In the case of NBD, nerves that control the bladder and muscles involved in urination cause the bladder to be overactive or underactive.
NBD symptoms may include:
- Limited or no voluntary control
- Involuntary urination
- Feel sudden urge to urinate
- Frequent bathroom visits
- Bladder does not completely empty
- Bladder overfills and pressure causes accidental leakage of urine
- Bladder is unable to hold urine
The brain and spinal cord are the central chains of command that transmit signals and messages to and from the bladder. Photo Source: 123RF.com.
Bladder Symptoms In Patients With Parkinsonism
Although the basal ganglia have been shown to have an effect on micturition reflexes in experimental animals, there are several possible causes of urinary symptoms in a patient with parkinsonism. These include a number of possible neurogenic causes depending on the exact underlying neurological diagnosis as well as local urological problems. In Parkinson’s disease bladder symptoms usually occur at an advanced stage of the disease and prostatic outflow obstruction should first be excluded in an elderly man. However, in a patient with severe urinary symptoms yet relatively mild parkinsonism a diagnosis of multiple system atrophy should be considered.
The onset of urogenital symptoms in MSA may precede overt neurological involvement by some years and in a study of the duration of symptoms, erectile dysfunction and bladder complaints began 45 years prior to the diagnosis and, on average, 2 years before more specific neurological symptoms appeared. Almost half the male patients had had a transurethral prostatectomy with a beneficial result in very few .
Because of the motor neuron loss in Onuf’s nucleus, changes of chronic reinnervation in the motor units of both sphincters may be demonstrated and sphincter EMG may be contributory in making the diagnosis . However, if this test is not available there are clinical urological criteria which may assist in recognizing patients with MSA and should make a urological surgeon cautious about operating .
Don’t Miss: What Do You Do For A Urinary Tract Infection