Get Effective Treatment With A Team Approach
Women need to know that there are many options available to reduce and sometimes eliminate pelvic organ prolapse. I encourage women not to accept their symptoms as milestones of motherhood or aging. With active research into advanced techniques and new developments each year, women should feel empowered to ask their doctors for the latest treatments for incontinence and pelvic discomfort.
Find out more about pelvic organ prolapse treatment today. request an appointment online.
Donât Miss: Do Probiotics Help Prevent Urinary Tract Infections
Other Treatments For Overactive Bladder
There are also many other treatment options available for overactive bladder which may work well for you. When you discuss your symptoms with our team, we may recommend some of these treatments to help you improve bladder control and symptoms.
For example, our providers may recommend lifestyle changes, such as maintaining a healthy weight to reduce the pressure on the bladder. We may also recommend Kegel exercises, which can strengthen the pelvic muscles. Also, scheduled bathroom breaks, even if you dont feel the urge to go, can help retrain your bladder to prevent those strong and sudden urges to urinate.
Other treatment options include medications. Typically, the medications are designed to relax the bladder to help with the symptoms of urgency. These often come in pills or patches you use each day. However, some people also receive small doses of Botox in the bladder to help relax the muscles. Our providers can discuss personalized treatment options for you.
What Can You Do
That depends on the type of incontinence you have, but small changes may help you regain control of your bladder.
Tighten your pelvic floor.Kegel exercises involve repeatedly tightening and releasing your pelvic floor muscles for a few seconds. You can get the idea of how to do them by stopping your urine, but dont do that routinely. If you block the flow of pee, it might lead to an infection. Aim to do three sets of 10 Kegels each day.
Watch what you drink. Coffee, tea, soda, and alcoholic drinks may cause your bladder to fill quickly, then leak.
Limit liquids later in the day. If you usually wake at night needing to go, cut back on the amount of fluids you drink during the evening.
Keep a healthy weight. Extra pounds put more pressure on your bladder.
Time your bathroom trips. If you make bathroom breaks on a set schedule — for instance, every hour — it can help you regain control of your bladder muscles. Once you see improvement, try slowly extending the time you head to the toilet.
Continued
Don’t Miss: How To Kill E Coli Bacteria In Urinary Tract
Treating And Managing Urinary Incontinence
Today, there are more treatments and ways to manage urinary incontinence than ever before. The choice of treatment depends on the type of bladder control problem you have, how serious it is, and what best fits your lifestyle. As a general rule, the simplest and safest treatments should be tried first.
A combination of treatments may help you get better control of your bladder. Your doctor may suggest you try the following:
The Lack Of Urinary Control

Have you ever asked, Why cant I hold my pee all of a sudden? A laugh. A cough. A sneeze. An exciting moment. These are things that many women grow to fear or become anxious about if they suffer from urinary incontinence. Some might consider these the lucky ones, especially those who dont only lose control during those moments, but also fear bladder leakage and the loss of urinary control at any moment.
There are many types of urinary incontinence such as urge incontinence, stress incontinence, functional incontinence, and reflex incontinence to name a few. Urinary incontinence affects 4 in 10 menopausal women in the US and is most likely due to the loss of estrogen. This decrease in estrogen weakens the urethra which helps to keep urine in the bladder. Estrogen is the main operating software for women, and with its decline after menopause comes a whole host of other issues ranging from heart disease to osteoporosis. Urinary incontinence, however, maybe one of the most damaging problems of menopause from a psychological point of view since it can cause constant anxiety, and can lead to moments of shame.
Estrogen Therapy Replacement as an Effective Form of Urinary Incontinence Treatment Fortunately, estrogen replacement therapies are effective forms of urinary incontinence treatment that can help alleviate symptoms caused by menopause, and maybe even get rid of it altogether. Choosing an appropriate estrogen, however, is an important step which is most often disregarded.
Also Check: How Can A Woman Get A Urinary Tract Infection
Vaginal Estrogen And Pelvic Floor Physical Therapy In Women With Symptomatic Mild Prolapse
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government.Know the risks and potential benefits of clinical studies and talk to your health care provider before participating. Read our disclaimer for details. |
| First Posted : July 24, 2012Last Update Posted : February 4, 2022 |
- Estrogen therapy in the previous year
- Current or prior breast or pelvic malignancy
- Contraindication to hormone use
Information from the National Library of Medicine
To learn more about this study, you or your doctor may contact the study research staff using the contact information provided by the sponsor.
Please refer to this study by its ClinicalTrials.gov identifier : NCT01648751
Dont Miss: Estrogen Positive Breast Cancer Recurrence
Assessment Of Risk Of Bias
Risk of bias was assessed using the Cochrane Risk of Bias Tool . We assessed the risk of bias of the studies that were published after the date of the search in the Cochrane reviews of Suckling , Cody or Ismail or studies that were not included in the Cochrane reviews but were considered relevant for our review. For the studies included in the Cochrane reviews we used the Cochrane authors assessment of risk of bias. Selection, data extraction and risk of bias assessment were performed by two reviewers independently. Disagreements were resolved by discussion, or if necessary, by a third reviewer.
Recommended Reading: Royal Canin Urinary So Calories
Cytokine Release And Viability Assay
CFT073 was grown in MSM in the presence of absence of estradiol statically at 37°C for 24 h. Estradiol was washed away from the bacteria with PBS and the bladder epithelial cell line 5,637 was infected with the respective treatment at MOI of 10 for 6 h at 37°C and 5% CO2. Supernatants were collected after the infection and centrifuged for 5 min at 5,000×g and stored at 80°C. An enzyme-linked immunosorbent assay was performed to measure IL-1 and IL-8 release from the 5,637 cells. The cytokine was measured with the IL-1 and IL-8 kits according to the instructions of the kit. Cell viability after infection was assessed by Pierce LDH cytotoxicity assay according to the instructions of the kit.
Vaginal Estrogen And Surgery
It is known that topical estrogen can treat age-related skin changes such as wrinkles and thin skin. Estrogen also increases the rate of cutaneous wound healing in older women and men. Estrogens act on the cutaneous wound healing response by modulating the inflammatory response, cytokine expression and matrix deposition. They also accelerate re-epithelialization, stimulating angiogenesis and wound contraction, and regulate proteolysis. While estrogens impact wound on healing of nonkeratinized vaginal epithelium remains to be described, its potential positive impact, currently adds to the rationale for perioperative use in vaginal surgery. There are no studies that directly compare the ease of the surgical procedure or its outcomes in women pretreated with intravaginal estrogen compared to those without treatment with intravaginal estrogen.
Recommended Reading: Urinary Tract Infection And Alcohol
You May Like: Is Urinary Tract Infection A Sexually Transmitted Disease
Menopause & Pelvic Organ Prolapse At A Glance
- Changes in a womans pelvic floor function often accompany menopause. Weakening of the pelvic support structures can lead to pelvic organ prolapse, in which one or more organs of the pelvic area drops out of place.
- While there are many causes of pelvic organ prolapse , the lack of estrogen during menopause thins the support structures and tissue that hold pelvic organs in place, causing them to fall.
Pelvic Floor Changes And Prolapse
The muscles and ligaments of the pelvic floor are all estrogen-sensitive, and changes in collagen, due to estrogen deficiency can have a profound effect on the support mechanisms of the pelvic floor.
The protective covering of the clitoris may be affected by changes in the urogenital tissue quality. The clitoris can become exposed and hypersensitive or buried underneath the fused labia minora.
Don’t Miss: How To Cure Urinary Tract Infection
Why Use Vaginal Estrogen Cream
There are many different treatments for symptoms of menopause and low estrogen available today. You could change your diet or lifestyle or even supplement with different products.
Women who are going through menopause experience a dramatic shift in their hormones. As the hormones change and stop monthly periods, they can also create some unpleasant vaginal symptoms, such as:
- Vaginal dryness
- Pain during sex due to lack of natural vaginal lubrication
- Painful urination
- Sudden and frequent need to urinate
Hormones affect vaginal health. During menopause, these same hormones shift, changing vaginal health as well.
Vaginal estrogen cream is used to treat the above-mentioned symptoms, as well as others. It should only be used as prescribed by your doctor. If you have any of the above symptoms and are going through menopause, talk to your doctor. They may want to run a few tests before prescribing a vaginal cream to help alleviate these symptoms.
Estradiol And Estrone Assays And Assessment Of Adherence
To determine systemic absorption of estrogen during the 6-week preoperative period of cream application, serum levels of estrone and 17-estradiol were assessed at baseline and on the morning of surgery using a highly sensitive liquid chromatography-tandem mass spectrometry assay. The chromatographic separation was performed on 150 Ã 2.0 mm Phenomenex Synergi 4Max-RP columns as previously described . The assay had previously been validated and, for E1, critical analyte concentration was 1.2 pg/mL with a detection limit of 3.5 pg/mL and a practical detection range of 3.5600 pg/mL functional assay sensitivity for E1 was less than 11.9 pg/mL. The intraassay coefficient of variation for E1 ranged from 9% at a concentration of 11.5 pg/mL to 2% at 365 pg/mL, whereas interassay CVs were between 12% and 4% . For E2, the critical concentration was 1.7 pg/mL with a lower detection limit of 2.8 pg/mL the detection range was 2.8600 pg/mL, and the functional sensitivity was 6.3 pg/mL. The intraassay CV ranged from 15% at a concentration of 6.6 pg/mL to 2% at 357 pg/mL interassay CVs were between 20% and 5% . Hysterectomy specimens were examined by a blinded pathologist for endometrial and myometrial thickness and pathology.
Read Also: Urinary Tract Infection And Treatment
Vaginal Atrophy: Vaginal Dryness Soreness And Painful Sex
Some women seek advice, but many dont ask for help for this under-recognised problem.
Management of urogenital atrophy
Some options that may help include:
- Avoidance of soaps to wash with
- Treatment of underlying skin problems with topical creams, often after guidance by a specialist and perhaps a skin-biopsy if required. These may include moistuising barrier creams and occasionally steroid ointment
- Regular use of vaginal moisturisers and lubricants
These treatments are effective and acceptable and unlike the conventional form of HRT, the effects are local, therefore the risk of systemic side effects are reduced.
Local estrogen therapy
Vulvovaginal dryness, soreness, burning, irritation, itching and chafing are likely to respond to local estrogen therapy, which can also help greatly with discomfort or pain during sex, correct the vaginal pH and prevent overgrowth of abnormal vaginal flora.
Estrogen delivered locally can be in the form of:
- Vaginal tablets, gel or a pessary all initially used daily, then twice weekly
- Creams: used daily initially, then twice weekly
- A vaginal silicone ring: changed 3 monthly
Selective Estrogen Receptor Modulator
Dehydroepiandrosterone 6.5mg
Vaginal Laser Treatment
How Is Low Estrogen Treated
Women who have low levels of estrogen may benefit from hormonal treatment. Hormonal treatment is the standard for low estrogen. There are non-hormonal options to help relieve symptoms. Non-hormonal options are preferred for women at high risk for breast cancer, blood clots, stroke, or liver disease.
Recommended Reading: Urinary Tract Burning Without Infection
How Does Low Estrogen Lead To Overactive Bladder
The link between overactive bladder and estrogen is complex. Researchers are still studying the exact cause. However, there are several potential explanations that may shed light on estrogens effects on the bladder.
Low estrogen can cause many changes in the body, including weaker pelvic muscles and a thinner urethra lining. These changes may increase the risk for overactive bladder and poor bladder control after menopause.
Dont Miss: Does Melatonin Help You Stay Asleep
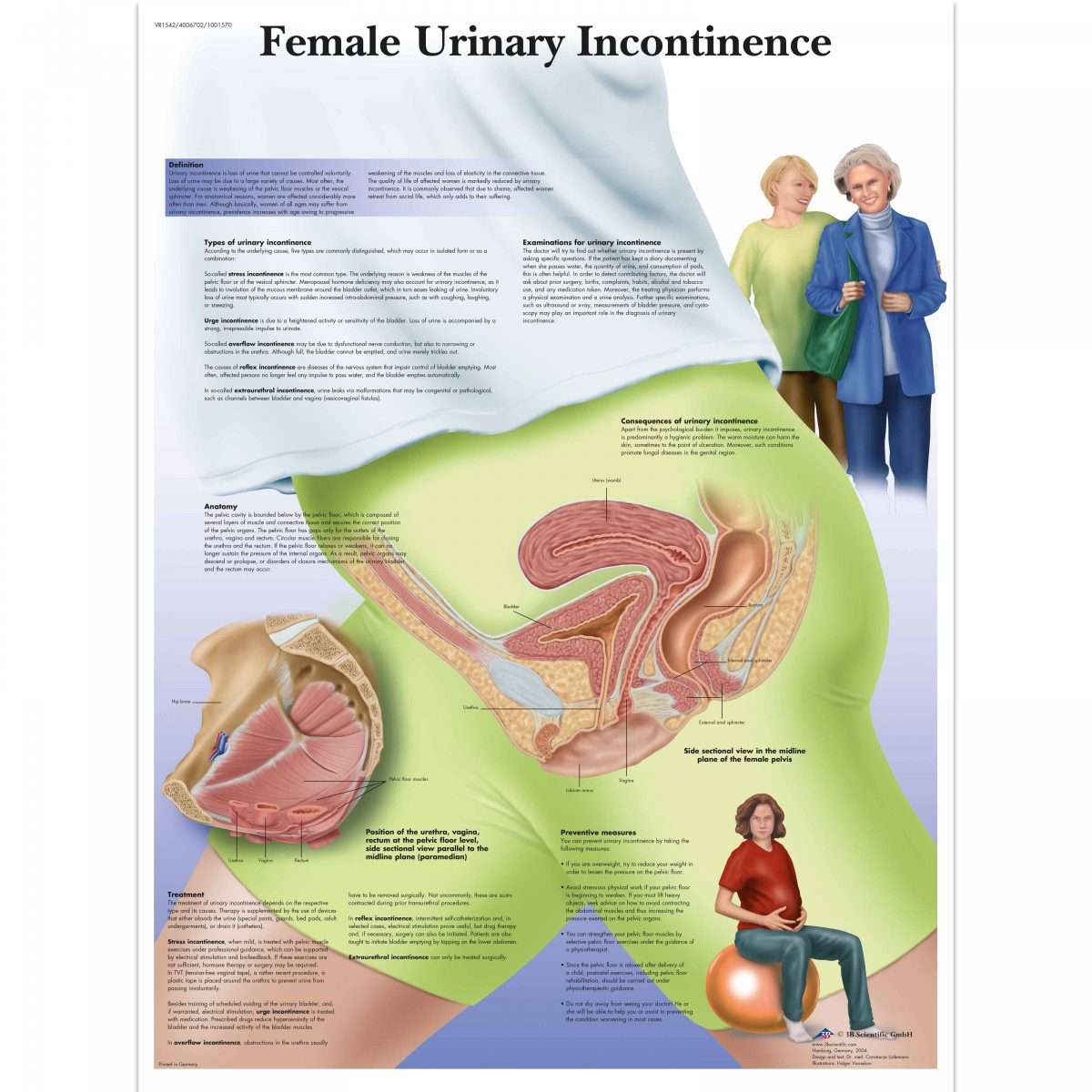
Types Of Urinary Incontinence
There are different types of incontinence:
- Stress incontinence occurs when urine leaks as pressure is put on the bladder, such as during exercise, coughing, sneezing, laughing, or lifting heavy objects. Its the most common type of bladder control problem in younger and middle-aged women. It also may begin later, around the time of menopause.
- Urge incontinence happens when people have a sudden need to urinate and cannot hold their urine long enough to get to the toilet. It may be a problem for people who have diabetes, Alzheimers disease, Parkinsons disease, multiple sclerosis, or stroke.
- Overflow incontinence happens when small amounts of urine leak from a bladder that is always full. A man can have trouble emptying his bladder if an enlarged prostate is blocking the urethra. Diabetes and spinal cord injuries can also cause this type of incontinence.
- Functional incontinence occurs in many older people who have normal bladder control. They just have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly.
Recommended Reading: Urinary Incontinence Treatment Home Remedies
What Is Considered Normal Bladder Function
- Passing urine 4-6 times per day
- Passing urine no more than once per night
- Passing 1-2 cups of urine each time
- Passing urine in a steady stream until the bladder is empty
- Being able to delay passing urine until convenient, and
- Having no leakage of urine between visits to the toilet
In a woman with normal bladder function, the muscles of the pelvic floor contract when she is doing any physical activities. These activities may include sneezing, coughing, sports or any other physical effort which can cause the pressure in the abdomen to rise.
When the pressure in the abdomen rises, the muscles of the pelvic floor contract, compressing the urethra and triggering contraction of the sphincter . This prevents any leakage of urine.
Learn How To Do A Proper Kegel Exercise
Watch Dr. Tran explain how to do a proper Kegel exercise:
Kegel exercises lessen stress incontinence in about half of patients, but the effect may not be noticeable until after 3-4 months of carrying out these exercises. Some other methods occasionally used to help with stress incontinence include vaginal Premarin cream and medicines to increase the tone of the urinary sphincter. Vaginal Premarin cream may improve the support of the bladder and urethra. Some of the drugs that can increase the strength of the urinary sphincter include Entex LA, Sudafed and Ornade.
If the above methods are unsuccessful and when the symptoms are troublesome enough that a patient wants something done, surgical re-suspension of the bladder and urethra can be carried out. Urethral slings are now the standard of care with 85-95% success rates typically. Complications of surgery can include bleeding and infection, in addition to the other general risks of surgery.
For some women with stress incontinence, the bladder and urethra are in the proper place but problems develop due to failure of the urethra to close tightly. In this case, collagen may be injected underneath the surface of the urethra to create a better seal. This technique is carried out on an outpatient basis with minimal sedation. As many as 75% of women notice a favorable improvement. Some women require re- treatment within several years if the collagen becomes reabsorbed.
Also Check: Urinary Tract Infection Go Away On Its Own
Reduced Cft073 Toxicity In The Presence Of Estradiol
We proceeded with evaluating the virulence of CFT073 in the presence of estradiol with an in vivo C. elegans infection model. This was done to evaluate the combined significance our findings had on the virulence of CFT073. We found that CFT073 in the presence of 5 and 300 pg/ml estradiol significantly increased the survival of C. elegans worms compared with unstimulated CFT073 . The dead worms were also visualized by the uptake of SYTOX Green . Estradiol per se did not induce any C. elegans toxicity .
Figure 8. CFT073 mediated C. elegans killing in the presence or absence of estradiol . Data are presented as mean ± SEM of n = 3 independent experiments. Statistical significance is denoted with asterisks: ***p< 0.001 vs. unstimulated CFT073. Immunofluorescence staining of dead worm with 1 M SYTOX Green . Scale bar: 1,000 m.
What Is Overactive Bladder
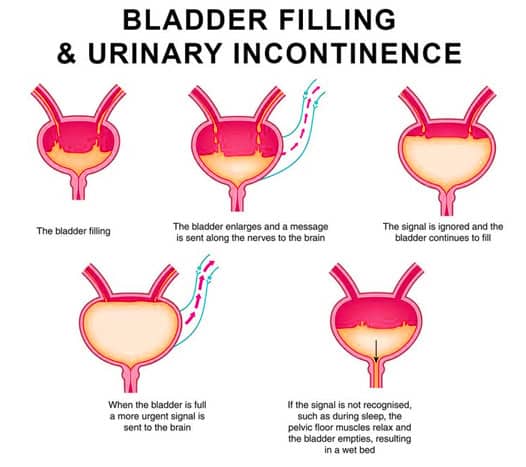
Overactive bladder is a health condition an estimated 33 million Americans experience. This condition affects your bladder control and can cause unwanted symptoms that affect everyday life. Overactive bladder is a type of urinary incontinence and is also known as urgency incontinence. OAB is different from stress incontinence, which can cause you to leak urine when theres extra pressure on your bladder, such as when you cough, sneeze, or laugh. Instead, overactive bladder generally means you experience frequent and urgent feeling that you need to pee, often at inconvenient times.
Read Also: Antiseptic For Urinary Tract Infection