How Do Healthcare Providers Diagnose Bladder Cancer
Healthcare providers do a series of tests to diagnose bladder cancer, including:
- Urinalysis: Providers use a variety of tests to analyze your pee. In this case, they may do urinalysis to rule out infection.
- Cytology: Providers examine cells under a microscope for signs of cancer.
- Cystoscopy: This is the primary test to identify and diagnose bladder cancer. For this test, providers use a pencil-sized lighted tube called a cystoscope to view the inside of your bladder and urethra. They may use a fluorescent dye and a special blue light that makes it easier to see cancer in your bladder. Providers may also take tissue samples while doing cystoscopies.
If urinalysis, cytology and cystoscopy results show you have bladder cancer, healthcare providers then do tests to learn more about the cancer, including:
Healthcare providers then use what they learn about the cancer to stage the disease. Staging cancer helps providers plan treatment and develop a potential prognosis or expected outcome.
Bladder cancer can be either early stage or invasive .
The stages range from TA to IV . In the earliest stages , the cancer is confined to the lining of your bladder or in the connective tissue just below the lining, but hasnt invaded the main muscle wall of your bladder.
Stages II to IV denote invasive cancer:
A more sophisticated and preferred staging system is TNM, which stands for tumor, node involvement and metastases. In this system:
History Of Prostate Cancer In The Era Of Prostate
based screening for prostate cancer led to earlier detection of prostate cancer , and thus altered the course of the disease in the absence of treatment . Identifying the incidence and prevalence of prostate cancer increased with widespread prostate-specific antigen testing, as did the length of time that men live with their disease, as compared to the pre prostate-specific antigen era. The stage migration that occurred, with application of curative intervention at an earlier stage, undoubtedly led to a reduction inprostate cancer mortality. However, the extent to which this reduction was due to prostate-specific antigen based screening is debatable. Further, because prostate cancer progresses slowly and is found most often in older men with competing risks of mortality, the extent to which these changes in natural history have resulted in benefit and harm are also debatable.
You May Like: Is Surgery The Best Option For Prostate Cancer
Patients May Want To Think About Taking Part In A Clinical Trial
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Also Check: Medicine For Male Urinary Tract Infection
Whats Usually The First Symptom Of Bladder Cancer
Blood in your pee is the most common bladder cancer symptom. That said, simply having blood in your pee isnt a sure sign of bladder cancer. Other conditions cause this issue, too. But you should contact a healthcare provider whenever you spot blood in your pee. Other bladder cancer symptoms include:
- Visible blood in your pee : Healthcare providers can also spot microscopic amounts of blood in pee when they do a urinalysis.
- Pain when you pee : This is a burning or stinging sensation that you may feel when you start to pee or after you pee. Men and DMAB may have pain in their penises before or after peeing.
- Needing to pee a lot: Frequent urination means youre peeing many times during a 24-hour period.
- Having trouble peeing: The flow of your pee may start and stop or the flow may not be as strong as usual.
- Persistent bladder infections: Bladder infections and bladder cancer symptoms have common symptoms. Contact your healthcare provider if you have a bladder infection that doesnt go away after treatment with antibiotics.
Treatment Of Stage I Bladder Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage I bladder cancer may include the following:
- Transurethral resection with fulguration. This may be followed by one of the following:
- Intravesicalchemotherapy given right after surgery.
- Intravesical chemotherapy given right after surgery and then regular treatments with intravesical BCG or intravesical chemotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
You May Like: Urinary Tract Infection After Menopause
Prognosis In Squamous Cell Carcinoma
Tumor stage, lymph node involvement, and tumor grade have been shown to be of independent prognostic value in SCC. However, pathologic stage is the most important prognostic factor. In one relatively large series of 154 cases, the overall 5-year survival rate was 56% for pT1 and 68% for pT2 tumors. However, the 5-year survival rate for pT3 and pT4 tumors was only 19%.
Several studies have demonstrated grading to be a significant morphologic parameter in SCC. In one series, 5-year survival rates for grade 1, 2, and 3 SCC was 62%, 52%, and 35%, respectively. In the same study of patients undergoing cystectomy, the investigators suggested that a higher number of newly formed blood vessels predicts unfavorable disease outcome.
In SCC, the survival rate appears to be better with radical surgery than with radiation therapy and/or chemotherapy. In locally advanced tumors, however, neoadjuvant radiation improves the outcome. Sex and age have not been prognostically significant in SCC.
Treating Stage Iv Bladder Cancer
These cancers have reached the pelvic or abdominal wall , may have spread to nearby lymph nodes , and/or have spread to distant parts of the body . Stage IV cancers are very hard to get rid of completely.
Chemotherapy is usually the first treatment if the cancer has not spread to distant parts of the body . The tumor is then rechecked. If it appears to be gone, chemo with or without radiation or cystectomy are options. If there are still signs of cancer in the bladder, chemo with or without radiation, changing to another kind of chemo, trying an immunotherapy drug, or cystectomy may be recommended.
Chemo is typically the first treatment when bladder cancer has spread to distant parts of the body . After this treatment the cancer is rechecked. If it looks like it’s gone, a boost of radiation to the bladder may be given or cystectomy might be done. If there are still signs of cancer, options might include chemo, radiation, both at the same time, or immunotherapy.
In most cases surgery cant remove all of the cancer, so treatment is usually aimed at slowing the cancers growth and spread to help people live longer and feel better. If surgery is a treatment option, it’s important to understand the goal of the operation whether it’s to try to cure the cancer, to help a person live longer, or to help prevent or relieve symptoms from the cancer.
Because treatment is unlikely to cure these cancers, many experts recommend taking part in a clinical trial.
Don’t Miss: Devices To Help With Urinary Incontinence
Search Page 1/: Urothelial Carcinoma Of Bladder
ICD-10-CM Diagnosis Code C67.0 Malignant neoplasm of trigone of bladder, Click on any term below to browse the neoplasms index. Papillary urothelial carcinoma Papillary carcinoma and Transitional cell carcinoma 8130 Renal Pelvis, local recurrence of malignant tumor of urinary bladder , high grade , which includes the renalThe ICD-10-CM code C67.9 might also be used to specify conditions or terms like adenocarcinoma of bladder, Ureter, It is
Dont Miss: Home Remedies For Urinary Urgency
How Can I Prevent Bladder Cancer
You may not be able to prevent bladder cancer, but it may be helpful to know the risk factors that may increase the chance youll develop bladder cancer. Bladder cancer risk factors may include:
- Smoking cigarettes: Cigarette smoking more than doubles the risk of developing bladder cancer. Smoking pipes and cigars or being exposed to second-hand smoke also increases that risk.
- Cancer treatments: Radiation therapy is the second-most common risk factor. People who have certain chemotherapy drugs may also develop an increased risk of bladder cancer.
- Exposure to certain chemicals: People who work with chemicals, such as aromatic amines , are at an increased risk. Extensive exposure to rubber, leather, some textiles, paint and hairdressing supplies, typically related to occupational exposure, also appears to increase the risk.
- Infections: People who have frequent bladder infections, bladder stones or other urinary tract diseases may have an increased risk of developing bladder cancer.
- Past bladder cancer: People with a previous bladder cancer are at increased risk to form new or recurrent bladder tumors.
Don’t Miss: Over The Counter Medicine For Urinary Urgency
Drg Mapping Rules For C670
Diagnostic codes are the first step in the DRG mapping process.
The patients primary diagnostic code is the most important. Assuming the patients primary diagnostic code is C67.0, look in the list below to see which MDCs Assignment of Diagnosis Codes is first. That is the MDC that the patient will be grouped into.
From there, check the subsections of the MDC listed. The patient will be mapped into the first subsection for which the treatment performed on the patient meet the listed requirements of that subsection.
DRG grouping rules are adjusted each year, so make sure to check the rules for the fiscal year of the patients discharge date.
Also Check: Best Med For Urinary Tract Infection
Looking For More Of An Introduction
If you would like more of an introduction, explore this related item. Please note that this link will take you to another section on Cancer.Net.
-
ASCO Answers Fact Sheet:Read a 1-page fact sheet that offers an introduction to bladder cancer. This free fact sheet is available as a PDF, so it is easy to print.
Also Check: Can Anxiety Cause Overactive Bladder
Also Check: Urinary Tract Infection Causes And Symptoms
Radiotherapy With A Radiosensitiser
Radiotherapy is given by a machine that beams the radiation at the bladder . Sessions are usually given on a daily basis for 5 days a week over the course of 4 to 7 weeks. Each session lasts for about 10 to 15 minutes.
A radiosensitiser should also be given alongside radiotherapy for muscle-invasive bladder cancer. This is a medicine which affects the cells of a tumour, to enhance the effect of radiotherapy. It has a much smaller effect on normal tissue.
As well as destroying cancerous cells, radiotherapy can also damage healthy cells, which means it can cause a number of side effects. These include:
- erectile dysfunction
- difficulty passing urine
Most of these side effects should pass a few weeks after your treatment finishes, although there’s a chance they’ll be permanent.
Having radiation directed at your pelvis usually means you’ll be infertile for the rest of your life. However, most people treated for bladder cancer are too old to have children, so this isn’t usually a problem.
After having radiotherapy for bladder cancer, you should be offered follow-up appointments every 3 months for the first 2 years, then every 6 months for the next 2 years, and every year after that. At these appointments, your bladder will be checked using a cystoscopy.
You may also be offered CT scans of your abdomen, pelvis and chest after 6 months, 1 year and 2 years. A CT scan of your urinary tract may be offered every year for 5 years.
Localized/early Transitional Cell Carcinomas Of Bladder
Transitional cell carcinomas can be very difficult to treat. Treatment for localized stage transitional cell carcinomas is surgical resection of the tumor, but recurrence is common. Some patients are given into the bladder either as a one-off dose in the immediate post-operative period or a few weeks after the surgery as a six dose regimen.
Localized/early transitional cell carcinomas can also be treated with infusions of into the bladder. These are given weekly for either 6 weeks or 3 weeks . Side effects include a small chance of developing systemic or the patient becoming sensitized to BCG, causing severe intolerance and a possible reduction in bladder volume due to scarring.
In patients with evidence of early muscular invasion, radical curative surgery in the form of a cysto-prostatectomy usually with lymph node sampling can also be performed. In such patients, a bowel loop is often used to create either a “neo-bladder” or an “ileal conduit” which act as a place for the storage of urine before it is evacuated from the body either via the urethra or a urostomy respectively.
Don’t Miss: Homeopathic Cure For Urinary Tract Infection
Permission To Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as NCIs PDQ cancer information summary about breast cancer prevention states the risks in the following way: .
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Bladder Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated < MM/DD/YYYY> . Available at: . Accessed < MM/DD/YYYY> .
Images in this summary are used with permission of the author, artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
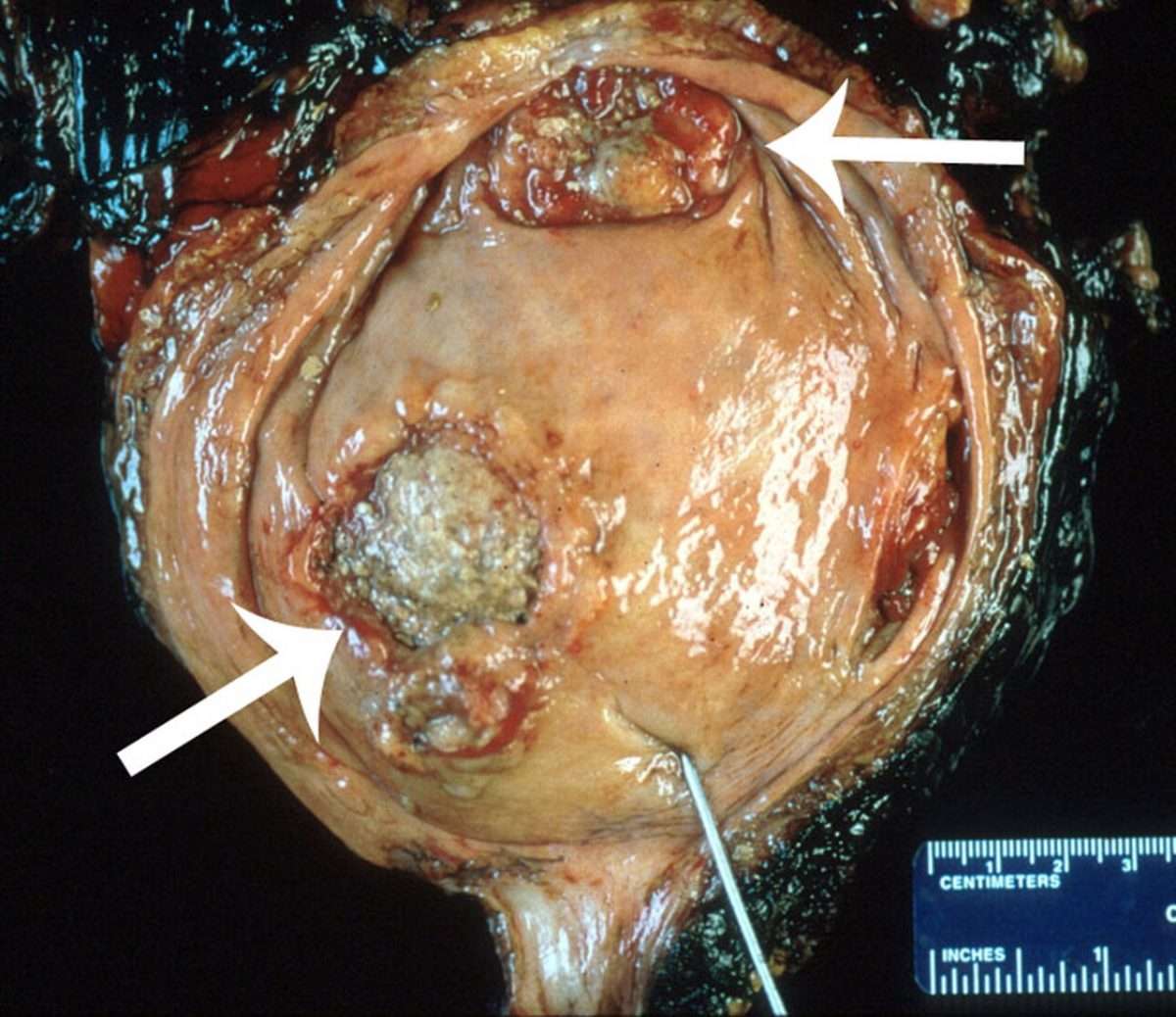
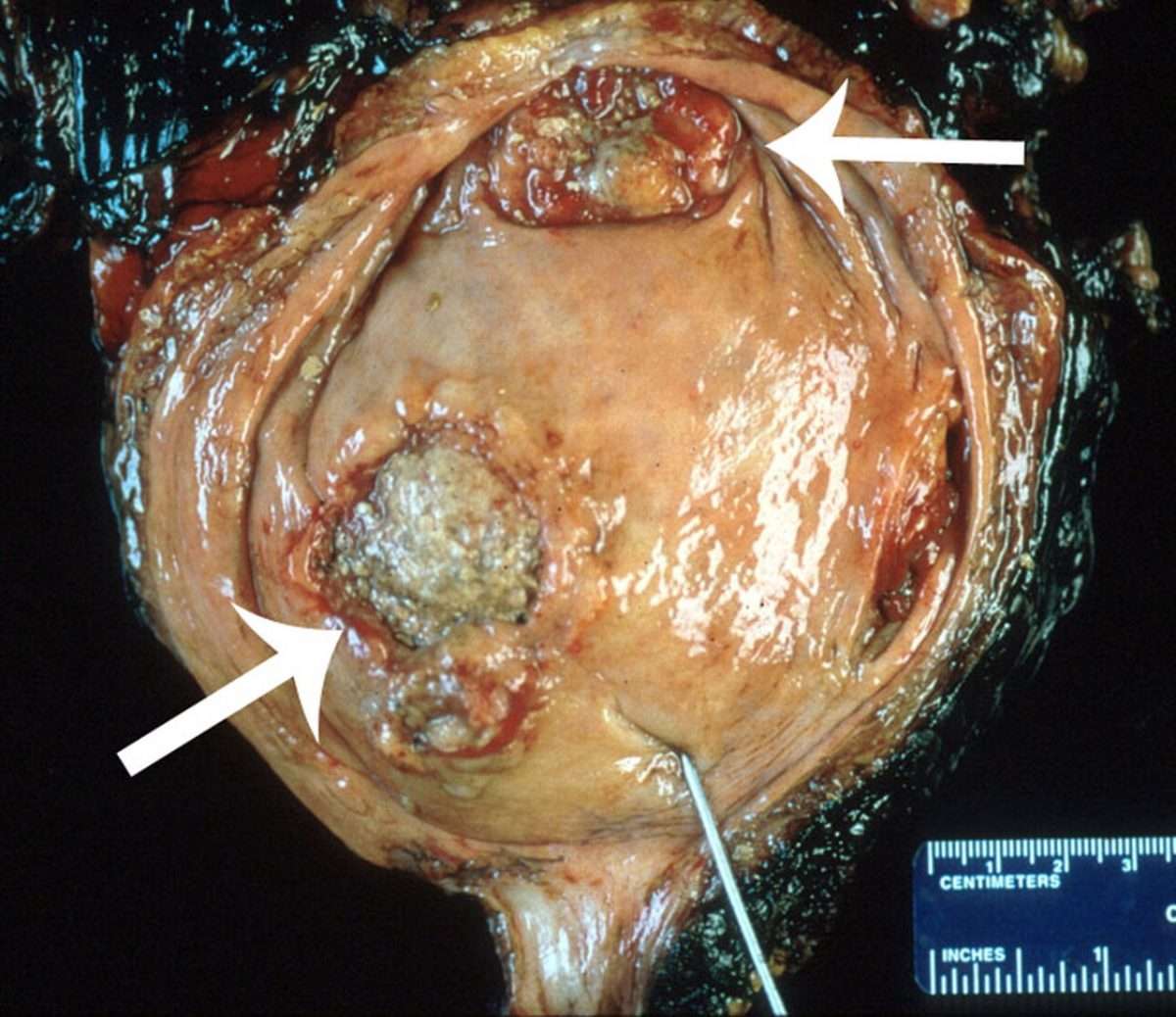
Cystectomy Cystoprostatectomy And Pelvic Exenteration Specimens
Proper fixation of the specimen is a prerequisite for adequate histological evaluation. We recommend that large bladder specimens be fixed in formalin overnight. Some prefer to expand the bladder with formalin. Injection of formalin into the urinary bladder cavity is accomplished either through the urethra by a Foley catheter or through the bladder dome using a large-gauge needle after the urethra has been clamped. We prefer to open the bladder before formalin fixation. It should be opened anteriorly from the urethra to the bladder dome. Thus the bladder mucosa may be everted for close examination. Any subtle alteration of the mucosa, such as granularity, ulceration, hemorrhage, or erythema, is documented. If a grossly visible tumor is identified, the size, location, configuration , color and consistency of the tumor should be documented.
The minimum number of sections to be taken are as follows: tumor bladder neck , trigone , anterior wall , posterior wall , lateral walls , dome , ureteral orifices , margins , any abnormal appearing bladder mucosa and any perivesical lymph nodes .
Figure 18
Illustration of a cystoprostatectomy specimen. Sections should be taken from tumor, bladder neck, trigone, anterior wall, posterior wall, lateral walls, dome, ureteral orifices , margins , and any abnormal appearing bladder mucosa. The prostate should be sampled using the standard protocol for radical prostatectomy specimens.
You May Like: How To Test For Urinary Incontinence
Malignant Neoplasm Of Bladder Unspecified C679
The ICD10 code for the diagnosis Malignant neoplasm of bladder, unspecified is C67.9. C67.9 is a VALID/BILLABLE ICD10 code, i.e it is valid for submission for HIPAA-covered transactions.
- C67.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2019 edition of ICD-10-CM C67.9 became effective on October 1, 2018.
- This is the American ICD-10-CM version of C67.9 other international versions of ICD-10 C67.9 may differ.
What Are The Signs Of These Types Of Tumors
The signs of urinary tract tumors depend on what area of the urinary system is affected. Tumors of the ureters, bladder, and urethra can cause hematuria , dysuria , difficulty urinating, and frequent urination. Recurrent and often unresolving secondary urinary tract infections are commonly associated with these types of tumors. If the tumor obstructs the ureter, preventing the flow of urine to the bladder, the kidney will swell with urine causing signs of abdominal pain. If the tumor obstructs the urethra, there may be lethargy, vomiting, diarrhea, straining or the inability to urinate.
The signs of urinary tract tumors depend on what area of the urinary system is affected.
Tumors of the kidneys can cause abdominal pain, blood in the urine, or non-specific signs such as lack of appetite, nausea or vomiting, weight loss, fever, lethargy, and swelling of the abdomen. Occasionally kidney tumors can cause increased urination and drinking.
Because many urinary tract tumors will spread to other areas in the body , there may be signs elsewhere . Kidney pain can sometimes be difficult to distinguish from back pain.
Read Also: Urinary Tract Infection After Period
Implications Future Research And Conclusions
In this population based cohort study, a first diagnosis of acute urinary retention was a clinical marker for occult cancer. We found that not only prostate cancer but also other urogenital, colorectal, and neurological cancers should be considered in patients aged 50 years or older who present with acute urinary retention and no obvious underlying cause. For most cancers, no excess risk was observed beyond three months of follow-up, suggesting that no major delay in cancer detection occurred. Whether the sustained increased risk of prostate and urinary tract cancers persisting for more than three months of follow-up represents an opportunity for earlier detection of these cancers remains to be elucidated and could be a focus for future research.
What is already known on this topic
-
Acute urinary retention might be a clinical marker of occult cancer
-
Existing evidence is sparse, of older age, and limited to data from only one institution
What this study adds
-
Acute urinary retention was found to be a clinical marker of prostate and other cancers
-
For most cancers, the excess cancer risk was confined to the first three months after a diagnosis of acute urinary retention
-
Occult cancer should possibly be considered in patients who present with acute urinary retention and no obvious underlying cause