How Is A Chronic Urinary Tract Infection Diagnosed
If you have a chronic UTI, you probably had a UTI in the past.
Performing lab tests on a sample of urine is the most common method doctors use to diagnose UTIs. A medical professional will examine the sample of urine under a microscope, looking for signs of bacteria.
In a urine culture test, a technician places a urine sample in a tube to encourage the growth of bacteria. After one to three days, theyll look at the bacteria to determine the best treatment.
If your doctor suspects kidney damage, they may order X-rays and kidney scans. These imaging devices take pictures of parts inside your body.
If you have recurring UTIs, your doctor may want to perform a cystoscopy. In this procedure, theyll use a cystoscope. Its a long, thin tube with a lens at the end used to look inside your urethra and bladder. Your doctor will look for any abnormalities or issues that could cause the UTI to keep coming back.
Youve Got A Cold The Flu Or Allergies
You may be tempted to curse your seasonal sneezes, a cold, or the dreaded flu for making your life even more miserable with a UTI, but these ailments arent the cause. The meds you take to manage symptoms could be.
Though theyre the bomb at keeping your runny or stuffy nose in check, antihistamines and decongestants might make you go less by causing urinary retention. And see No. 6 that may lead to a UTI.
I Feel Like I Have A Uti But My Tests Are Negative
Sound familiar? Unfortunately the standard tests used to diagnose UTIs dipstick tests and mid-stream urine cultures miss about half of infections. The figure is likely to be even higher for chronic infections.
But some doctors are more likely to rely on test results than on the symptoms their patients are describing and rule out infection as a cause.
No test is perfect, as they all have different sensitivity levels. A relatively low concentration of bacteria may fall below the sensitivity limit of a given test, but still be concentrated enough to have a profound effect on the patient. As a result, UTIs are best diagnosed with a combination of tests, physical examinations and symptom analysis.
Also Check: Z Pak For Urinary Tract Infection
The Myth Of Interstitial Cystitis And Bladder Syndromes
IC and bladder syndromes are known as diagnoses by exclusion. They dont identify a reason for a patients symptoms, they simply describe collections of symptoms. For example, the NHS Choices website describes IC as a poorly understood, incurable condition.
There is no agreed cause or cure for IC and bladder syndromes. But there is a view among many doctors based on tests which are known to be ineffective that they are not caused by bacteria. Sufferers are offered surgery or prescribed painkillers, including opiates, bladder relaxants and bladder instillations to alleviate symptoms.
Bladder instillations had no more effect than a placebo, a recent large-scale study found. A growing body of evidence suggests that long-term bladder and urinary pain may be caused by infections missed by tests that dont work.
Can You Test For Biofilms In The Bladder
The presence of biofilms in the bladder is not far-fetched science.
The National Institutes of Health estimates around 80% of all bacterial infections in humans involve biofilms.
Although the existence of biofilms in human infection has been accepted in medicine for decades, it is much more recently that attention has turned to their involvement in chronic UTI.
| In my opinion it’s pretty clear that biofilms and IBCs are a true phenomenon, and it would explain why a given patient can get what seems like a perfectly appropriate antibiotic based on antibiotic susceptibility testing from cultured bacteria. Then as soon they stop taking the antibiotic, the same exact bacterial isolate comes roaring back with the same antibiotic susceptibility. Why wasnt it wiped out? Well, I think sometimes it’s IBCs, or biofilms. And then in other cases, it may be that they’ve reseeded themselves from their distal guts or their vagina as well.” |
Traditionally, testing labs have focused on culturing and testing free-floating pathogens. If free-floating pathogens are identified, their susceptibility to antibiotics is also tested while they are in a free-floating state.
Once the susceptibility has been tested, it is possible to prescribe the right treatment.
The problem with these types of tests is that they do not specifically detect biofilm formations in the bladder. And therefore, they are not helpful in deciphering which treatments may be effective against microbes within a biofilm.
Recommended Reading: Why Do You Keep Getting Urinary Tract Infections
Risk Factors And Pathophysiology
A variety of risk factors predispose LTC residents to developing UTIs. Patient risk factors result from a combination of physiological changes of aging and accumulation of comorbidities. Aging disrupts acquired immunity because of T-cell dysfunction and blunted cytokine-mediated inflammatory response. This impaired cellular function is accentuated in the setting of diabetes, cancer, and autoimmune disorders. In addition, comorbidities result in bladder and bowel incontinence and functional decline, all of which disrupt the bodys innate defense mechanisms.- In women, estrogen deficiency can cause vaginal prolapse and urinary incontinence, promoting an ascending flow of bacteria to the sterile urinary tract. Estrogen deficiency also impairs the protective action of bacterial colonization of the vagina with Lactobacillus, which normally suppresses the growth of pathogenic bacteria. In older men, hypertrophy of the prostate causes urinary retention and turbulent urine flow, predisposing them to chronic prostatitis. The chronically inflamed prostate can form calculi that entrap bacteria, causing recurrent UTIs. In contrast to increased postvoid residual in community-dwelling older adults, however, this condition in LTC residents is not associated with an increased rate of UTIs.,
How Are Recurrent Utis Treated
Treatment for recurrent UTIs depends on what’s causing them. Sometimes the answer is as simple as teaching a child to empty their bladder as soon as they have the urge to go.
If a condition like VUR is causing the infections, the solution is a bit more complicated. Kids with VUR must be watched closely, because it can lead to kidney infection and kidney damage. Most kids outgrow the condition. Some might need surgery to correct the reflux.
Some kids with VUR benefit from daily treatment with a small amount of antibiotics, which can also make surgery unnecessary. Kids with VUR should see a pediatric urologist, who can decide if antibiotic treatment is the best option.
In some cases, surgery is needed to correct VUR. The most common procedure is ureteral reimplantation, in which one or both of the ureters are repositioned to correct the backflow of urine from the bladder. This procedure requires only a small incision and, in some children, can be done using robotic-assisted laparoscopy. When surgery is necessary, the success rate is high, but not everyone is a good candidate for it.
Kids may be candidates for ureteral reimplantation if they:
- have an intolerance to antibiotics
- get recurrent infections while on antibiotic treatment
- have severe, or “high-grade,” reflux
- are older kids and teens with reflux
You May Like: Pomegranate Juice For Urinary Tract Infection
How Do I Know If The Treatment Isnt Working
If the treatment isnt working, your symptoms will stay the same, get worse, or you will develop new symptoms. Call your doctor if you have a fever , chills, lower stomach pain, nausea, and vomiting. You should also call your doctor if, after taking medicine for 3 days, you still have a burning feeling when you urinate. If you are pregnant, you should also call your doctor if you have any contractions.
Chronic Urinary Tract Infection Causes
Urinary tract infections result from bacteria finding its way into your urine. Although urine is normally bacteria-free, there are many ways bacteria can enter your urinary tract. Causes and risk factors include:
- Sexual intercourse
- Certain types of birth control
- Low estrogen levels
- Holding in urine or not emptying your bladder completely
- Not drinking enough water
You May Like: Urinary Incontinence Devices For Women
Can I Become Immune To The Antibiotics Used To Treat A Uti
Your body can actually get used to the antibiotics typically used to treat a urinary tract infection . This happens in people who have very frequent infections. With each UTI and use of antibiotics to treat it, the infection adapts and becomes harder to fight. This is called an antibiotic-resistant infection. Because of this, your healthcare provider may suggest alternative treatments if you have frequent UTIs. These could include:
- Waiting: Your provider may suggest that you watch your symptoms and wait. During this time, you may be encouraged to drink plenty of fluids in an effort to flush out your system.
- Intravenous treatment: In some very complicated cases, where the UTI is resistant to antibiotics or the infection has moved to your kidneys, you may need to be treated in the hospital. The medicine will be given to you directly in your vein . Once youre home, you will be prescribed antibiotics for a period of time to fully get rid of the infection.
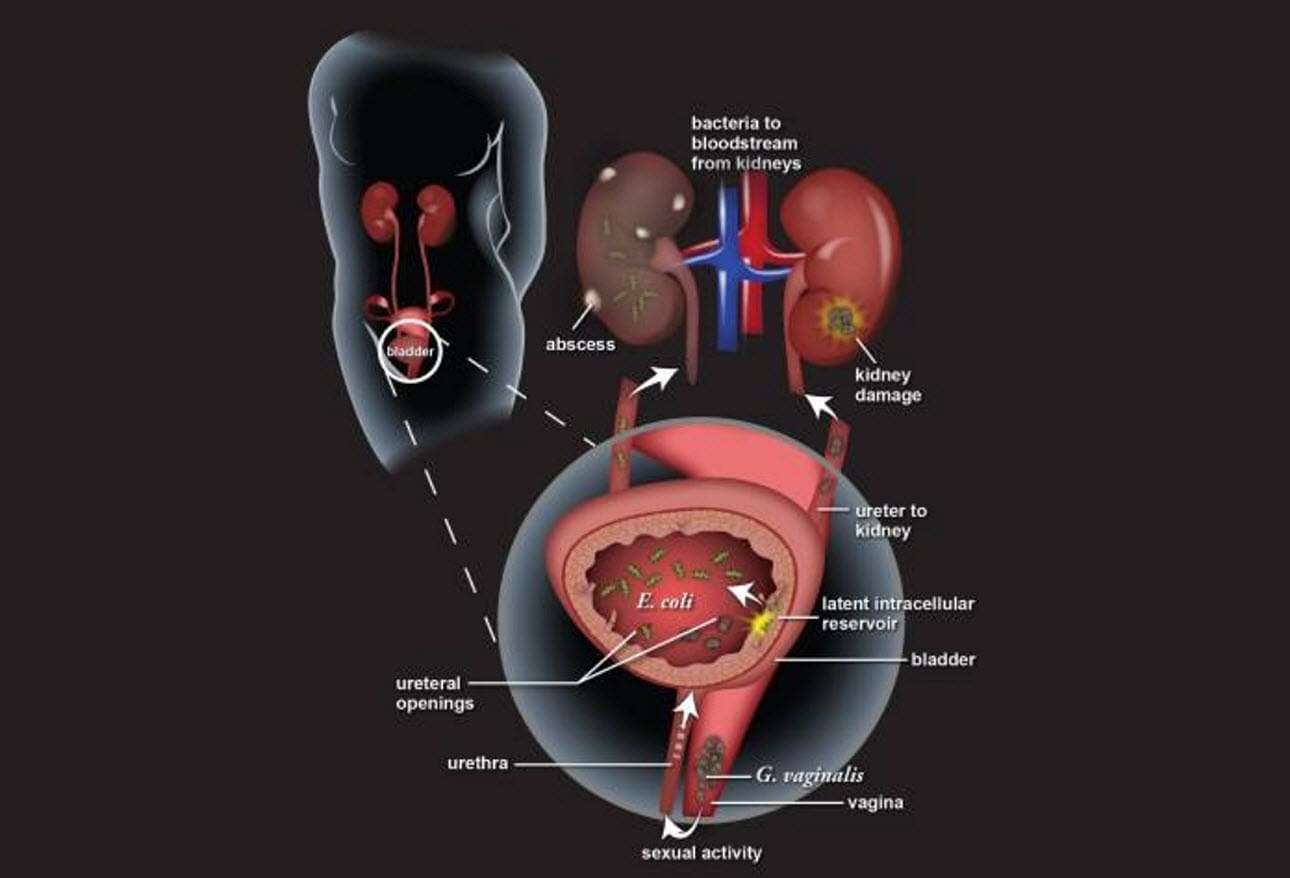
What Causes Urinary Tract Infection
The vast majority of urinary tract infections are caused by the bacteria Escherichia coli , which is usually found in the digestive system. However, other pathogens may cause a UTI. These include:
- Klebsiella pneumonia
- Enterococcus faecalis
- Staphylococcus saprophyticus
The bacteria may infect any part of the urinary tract bladder, urethra or kidneys. Depending on where the infection occurs, the UTIs are often known as:
- Cystitis infection of the bladder
- Urethritis infection of the urethra
- Pyelonephritis infection of the kidneys
The infection in urethra and bladder is usually not very serious and clears up with treatment. Similarly, ureters very rarely get infected. However, if a UTI reaches the kidneys, it may lead to kidney infections and a person may have to go to the hospital for treatment.
Recommended Reading: What Is Urinary Tract Health
You Dont Pee After Sex
The threat of getting a UTI shouldnt stop you from getting it on. But that doesnt mean resigning yourself to the afterburn.
One simple way to cut your risk: Head to the potty after youve finished your romp. Youll possibly flush out the bacteria that may have made their way into your urinary tract. Urinary Tract Infection. .
Why Does My Uti Keep Coming Back
Chronic or recurring UTIs may keep coming back due to one of the risk factors listed above. Use of spermicides for birth control, for instance, may kill off beneficial bacteria in and around the vagina, making it easier for harmful bacteria to enter the urinary tract.
In some cases, what seem like recurrent UTIs may actually be another condition, such as kidney stones or interstitial cystitis, a painful bladder condition with no infection. If you think youre getting recurrent UTIs, see your provider, who can help rule out another condition, notes ACOG.
Read Also: Can I Use Azithromycin For Urinary Tract Infection
Does Cranberry Juice Prevent A Urinary Tract Infection
Many people say that cranberry juice can help treat, or even prevent, a UTI. Researchers are currently looking into the topic, but havent found a definitive answer yet. Healthcare providers recommend drinking lots of fluids if you have, or have a history of getting, a UTI. Adding a glass of unsweetened cranberry juice to your diet isnt a proven way to prevent a UTI, but it typically wont hurt you either.
How Does A Chronic Uti Start
A chronic UTI starts with an acute infection that doesnt get better or seems to clear up but comes back repeatedly. Short courses of between one to three days are too short to clear infection and symptoms return a few days after finishing the course of antibiotics.
Needing to pee all the time, pain when you pee, passing tiny amounts of urine, bladder and urethral pain, pain in your belly, back and legs, difficulty passing urine, problems with incontinence. The symptoms of chronic UTI are similar to acute infections but they vary from person to person.
Its not clear why some people suffer from chronic infections while others get better. But what is known is that chronic UTIs wreck lives. Sufferers are left with debilitating, life-changing symptoms including urinary frequency , urinary urgency, agonizing pain, unable to sleep properly, work, look after children and have normal sexual relationships. Their lives grind to a halt.
Also Check: Tips For Urinary Tract Infection
How Does An Infection Become Chronic
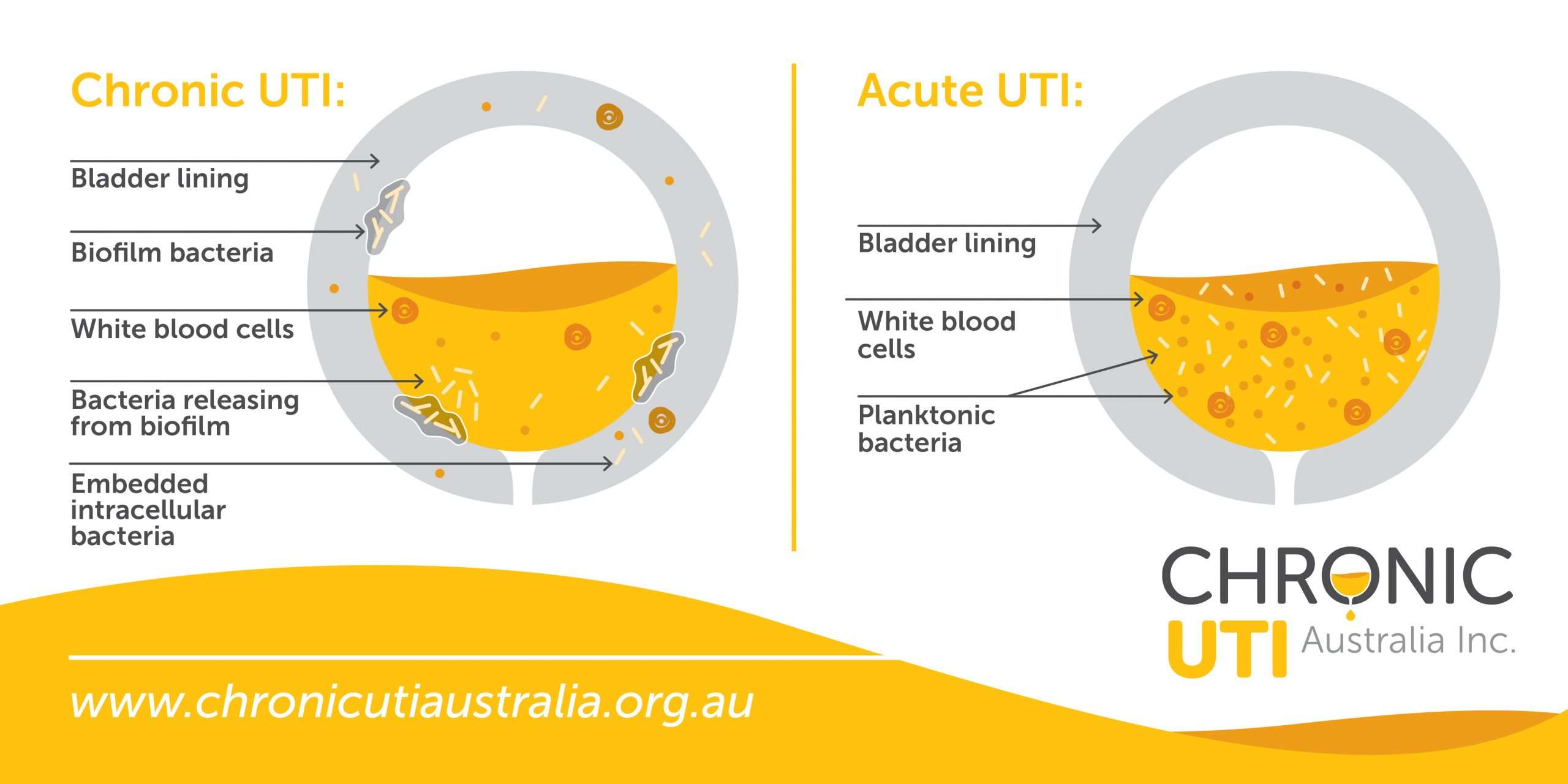
Chronic UTIs develop when acute or simple infections are left untreated or fail to get better with standard treatments such as over-the-counter remedies or the short courses of antibiotics that GPs usually prescribe.Over time the bacteria that cause UTIs move from the urine and into the cells of the bladder wall where they are protected from antibiotics and become harder to kill. Bacteria cause the bladder cells to become inflamed. This allows the bacteria to stick to the tissues and become harder to flush out.
We explain how a chronic UTI develops brought to life with some great images.
Persistent Uti Vs Recurrent Or Frequent Uti: Whats The Difference
| A recurrent urinary tract infection is officially defined as three episodes of a UTI in the previous 12 months or two episodes within the previous 6 months. |
At the moment, it is generally accepted that recurrent UTIs occur due to either reinfection or a persistent infection.
| Reinfection refers to an infection where the pathogen is eradicated by treatment, then the same or a different pathogen ascends the urinary tract to cause a new infection. |
| Persistence means the pathogen that caused the UTI is not completely cleared from the bladder by treatment, remains detectable in the urine, and after treatment returns to a level that once again causes symptoms of infection. This cycle of persistence can repeat indefinitely, feeling like a new infection each time. A persistent infection is also called a chronic urinary tract infection. |
Evidence suggests that many recurrences of UTI may actually be caused by an underlying bladder infection that came about due to ineffective initial treatment.
Frequent UTIs caused by persistent bladder infection are also referred to as chronic cystitis or chronic urinary tract infection.
Note that while terms used for various urinary tract conditions may sound different, they could refer to the same thing.
When we refer to recurrent UTI in this site, we usually mean persistent infections also called chronic urinary tract infections.
Whatever youre doing to treat each occurrence of UTI is probably not working.
You May Like: Where To Buy Azo Urinary Pain Relief
Other Ways To Prevent Recurring Utis
If you have more than 3 UTIs in 1 year, or 2 UTIs in 6 months, there are other things that may help prevent UTIs.
There is some evidence that women under 65 years old who keep getting UTIs may find it helpful to take:
- a supplement called D-mannose this is not recommended for pregnant women
- cranberry products, such as juice or tablets
Speak to your doctor before taking any of these during pregnancy.
Be aware that D-mannose and cranberry products can contain a lot of sugar.
Page last reviewed: 18 November 2020 Next review due: 18 November 2023
Talking To Your Doctor
No detail is too small when visiting the doctor about urinary problems. We suggest you write down a list of symptoms and take them with you to your appointment. For example, an unusual smell, abnormal amounts of foam, or persistently darker urine than usual may seem unimportant to you, but to a doctor these can be the characteristic symptoms required to diagnose a given condition. Other signs to look out for and mention to your GP include:
- a weak or intermittent urinary stream
- straining
- nocturia getting up at night to urinate
- posturination dribbling
- pain or a stinging sensation in the urethra or penis whilst urinating or post urination.
- Pain radiating into the rectum
One major fear is that of a physical exam, especially when it relates to intimate parts of the body. A physical exam is likely to occur, so prepare yourself ahead of time for it. Do not be afraid to ask for a male doctor when making your appointment . A chaperone is also acceptable, and in some cases encouraged.
However, a doctor may not wish to examine you in certain conditions in these cases, do not be afraid to ask for one if you feel it necessary or would like to put your mind at rest. For example, younger men that present urinary symptoms will likely be assumed to not have prostatic issues and thus a doctor will likely not perform an exam. This doesnt exclude their presence entirely, so should you have any doubt it is recommended that you ask for the exam to be performed anyway.
Recommended Reading: Symptoms Of Pinworms In Urinary Tract
Embedded Or Biofilm Infection
When bacteria first enter the urinary tract, they are free-floating . However, under the right circumstances, these bacteria can stick to the bladder lining, and form a networked community, shielded by a protective slimy material. This slimy material protects the bacteria from antibiotics, as well as shielding it from the bodys natural defences. This is known as biofilm and can allow bacteria to survive for long periods. Once such a biofilm develops, whenever you get a UTI, instead of recovering completely, your body can be left with an embedded infection adherent to bladder wall, that is difficult to treat.
In addition to biofilms attached to the bladder wall, bacteria can also invade bladder cells and then rapidly replicate within the cells to form intracellular bacterial communities with enhanced resistance to antibiotics. However, within hours of IBC development, the progeny of successfully invasive bacteria emerge from the bladder cells, again in a free-floating state, ready to invade neighbouring cells to start the cycle anew. This form of invasion and intracellular replication affords a survival advantage for the bacteria to persist within the bladder as it sheds it lining.
Only in the last 10-15 years have biofilms and intracellular bacterial communities been recognised as a contributor to chronic bladder infection. Fortunately, research is now throwing further light on these mechanism and potential treatments to combat them.