Sphincterotomy And Urethral Stents
Though the first results with urethral stent as an alternative to conventional endoscopic sphincterotomy seemed promising , long-term results were not as satisfactory. Common complications are device migration, bladder neck obstruction, intravesical stone formation, encrustation, granulation tissue ingrowth, increase in AD and obstruction . A temporary stent can be used in patients planning fertility treatment or in patients where the consequences of eventual sphincterotomy need to be better explored.
Is Incontinence Normal After Prostate Surgery
Bladder leakage after prostate removal is not all that uncommon and typically will go away after your body begins to heal and your muscles regain strength. Approximately 6-8 percent of men who have had surgery to remove their prostate will develop urinary incontinence. The good news is that most men will eventually regain bladder control with time.
Neurogenic Bladder Disorder Is This Only A Problem Of The Lumbar Spine Is Your Cervical Spine The Cause
It is not easy to find research connecting cervical spine instability with urinary incontinence. We are going to see this below. The great weight of research centers on the problems of the lumbar spine and the neurological defects herniated lumbar discs may cause. But, as we will suggest and demonstrate, there is a connection between the cervical spine and urinary incontinence.
You May Like: Urinary Sepsis Symptoms In Elderly
Nearly Half Of All Patients Undergoing Elective Cervical Spine Surgery Had Moderate
Numbers:
- The prevalence of moderate lower urinary tract symptoms in the patient sample was 40%
- The prevalence of severe lower urinary tract symptoms in the patient sample was 8%
- Clinically relevant urinary bother was reported in 18% of patients
- The odds of moderate-to-severe lower urinary tract symptoms among patients with myelopathy were greater than that observed in patients without myelopathy
- The prevalence of clinically relevant urinary bother was higher in patients with myelopathy compared with those with no myelopathy .
Nearly half of all patients undergoing elective cervical spine surgery had moderate-to-severe lower urinary tract symptoms. This is more than double the prevalence that has been reported in a community-dwelling adult population. These symptoms can impair quality of life, lead to surgical complications , and may be mistaken for cauda equina , prompting potentially unnecessary imaging and studies.
Dr. Albert also suggested:
How Is Neurogenic Bladder Diagnosed
If your healthcare provider thinks you may have neurogenic bladder, he or she will want to check youre your brain, spinal cord, and bladder. He or she will review your health history and do a physical exam. Other tests may include:
- X-rays of the skull and spine. This imaging test uses invisible energy beams to make images of tissues, bones, and organs.
- Imaging tests of the bladder and ureters
- Ultrasound . This imaging test uses high-frequency sound waves to create images of the organs on a computer screen.
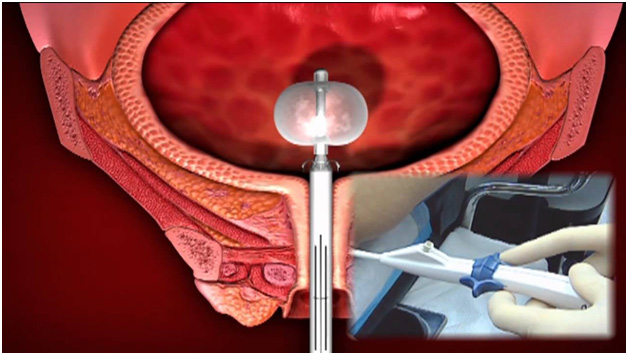
- Cystoscopy. Your healthcare provider puts a thin, flexible tube and viewing device in through the urethra to examine the urinary tract. It checks for structure changes or blockages, such as tumors or stones.
- Tests that involve filling the bladder, such as urodynamics. These tests show how much the bladder can hold and check to see if it fully empties.
Read Also: E Coli In Urinary Tract
How Can I Prevent Cauda Equina Syndrome
It may not be possible to prevent all of the causes of cauda equina syndrome. But, you might be able to reduce your risk of a herniated disk, the most common cause of the syndrome. Try the following tips:
- Avoid wearing high-heeled shoes. These types of shoes can misalign your spine.
- Stop smoking. Avoid using other tobacco products as well because they can weaken your disks.
- Exercise. Try exercises that strengthen your back and abdominal muscles.
- Lift properly. Bend your knees and keep your back straight when you lift something instead of bending at your waist.
- Maintain a healthy weight. Extra weight adds extra pressure to your lower back.
- Practice good posture. That will reduce strain on your spine.
- Stretch. Stretch your body periodically, especially after youve been sitting for a long time.
Category: Minimally Invasive Surgery Surgery Recovery
When a patient is experiencing bowel or bladder control loss, minimally invasive spine surgery can often be an effective treatment option for returning control to the patient. However, sometimes patients experience bowel and bladder issues after their minimally invasive spine procedure. Here, we will explain the various potential bladder and bowel issues that can impact a patient following a spine surgery, and offer tips for correcting these issues.
Also Check: Why Are Urinary Tract Infections Common In Older Adults
How Do I Take Care Of Myself
The best thing you can do for yourself if you have symptoms is to see a healthcare provider. Continue getting help from healthcare providers after you have surgery, including:
- Physical therapists.
- Primary care healthcare providers.
- Psychiatrists.
See if your family and friends are willing to help you as well. Youll need support.
Is Urinary Incontinence Normal After Hysterectomy
The most common after-hysterectomy problem is pelvic floor dysfunction. However, the most common type of pelvic floor dysfunction is urinary incontinence, and often after the surgery. But not all women suffer from it only about 30% or so experience one or more symptoms of post-surgical SUI/stress voiding.
Hysterectomy does not cause urinary incontinence. Loss of support for the bladder neck and urethra is what causes it.
The incidence of urinary incontinence after hysterectomy varies depending on which surgical technique is used. The highest incidence is after vaginal hysterectomies because these procedures disrupt supporting structures of the bladder more than abdominal procedures.
About half of patients who have vaginal hysterectomy experience urinary incontinence after their surgery, most often due to injury to the urethra or bladder neck during the procedure.
After an abdominal hysterectomy, about 10-20 percent of women will experience stress-related urinary incontinence, but the risk seems to increase to 40-50 percent when combined with other pelvic surgery such as bladder or vaginal surgery.
Don’t Miss: Can Humira Cause Urinary Tract Infections
The Long Term Outcome Of Micturition Defecation And Sexual Function After Spinal Surgery For Cauda Equina Syndrome
-
Affiliation Department of Neurosurgery, Leiden University Medical Center, Leiden, the Netherlands
-
Affiliations Department of Neurosurgery, Leiden University Medical Center, Leiden, the Netherlands, Department of Neurosurgery, Haaglanden Medical Center, the Hague, the Netherlands
-
Affiliation Department of Neurosurgery, Leiden University Medical Center, Leiden, the Netherlands
Urologic Symptoms Of Neurodegenerative Disorders
The urologic manifestations of neurodegenerative disorders, including Parkinson disease , multisystem atrophy, and Huntington chorea, have been studied by several groups.
Brusa et al showed that initiation of L-dopa therapy worsened bladder overactivity and reduced capacity, but long-term use improved sensation of bladder filling and capacity.
These investigators also reported impaired relaxation of the external urethral sphincter and the presence of Lewy bodies in the colonic mesenteric plexus. The degree of sphincteric involvement appears to be a function of autonomic involvement.
Patients with multisystem atrophy and autonomic failure have considerable difficulty with incontinence. Sphincter EMG of these patients has shown abnormal motor units and increased motor unit durations. Patients with multisystem atrophy and Shy-Drager syndrome are known to have cell loss in the motor nuclei at S2-S4 this finding has led to increased speculation concerning the autonomic properties of these neurons.
Paviour et al reviewed 37 patients with multisystem atrophy who underwent sphincter EMG and concluded that the changes seen were not specific.
The incontinence in Huntington chorea and in other dementing illnesses is synergic loss of urine caused by the loss of central inhibitory pathways. Normal or near-normal sphincter activity is preserved in most disorders of muscle or anterior horn cells.
You May Like: How To Treat Urge Urinary Incontinence
How Is It Managed
If you experience difficulty urinating or completely emptying your bladder after surgery, make sure you let the doctor or nurse know. Chances are, they will ask if you have passed urine or are having difficulty. In the majority of cases, the problem will resolve itself with a bit of time, but if the bladder is full and wont release, a catheter will be inserted, and the urine drained. Patients arent discharged until the matter is satisfactorily resolved.
People Getting Cervical Spine Surgery Already Have Urinary And Bladder Problems
In April 2019, doctors at the Department of Orthopaedics and Rehabilitation, Oregon Health & Science University published their research findings that made a connection between lower urinary tract symptoms and urinary bother in patients who underwent elective cervical spine surgery. The research was published in the journal Clinical Orthopaedics and Related Research.
The researchers record that the purpose of this study was to:
The research:
- 242 patients (youngest 34 to oldest 83 years average group age 58
- There were 108 males and 134 females .
- Patients were grouped into a myelopathy group and a non-myelopathy group based on diagnosis as assigned by the operating surgeon.
Read Also: Do You Get A Fever With A Urinary Tract Infection
How Is Cauda Equina Syndrome Diagnosed
Your healthcare provider will diagnose your cauda equina syndrome by interviewing you about your symptoms, assessing your physical abilities, performing tests and ordering imaging tests. Theyll assess your abilities by having you:
- Displaced spinal cord or nerves because of herniated disks, bone spurs and tumors.
Youll be diagnosed with cauda equina syndrome if you have two sets of symptoms:
- Bowel, bladder and/or sexual problems.
- Paresthesia of the backs of your legs, butt, hip and inner thighs.
Why Prostate Surgery Causes Incontinence
Your bladder stores urine until your brain signals its time to release it. The urethra is a tube that transports urine from your bladder to the outside of your body. There are two valves, called sphincters, on your urethra that open to release urine.
Your prostate gland surrounds your urethra and is located near one of those sphincters, and when you have your prostate removed, one of your sphincters is removed as well. Most of the time, having one functioning valve to hold in or release urine may be sufficient, but in some cases the nerves and muscles in the area are affected and urinary incontinence is the result. Prostate removal surgery may include complete removal for cancer or partial removal to treat an enlarged prostate.
Don’t Miss: How To Ease Urinary Tract Infection Pain
Botulinum Toxin A Injections
Botulinum toxin A can be injected into the sides of your bladder to treat urge incontinence and overactive bladder syndrome.
This medicine can sometimes help relieve these problems by relaxing your bladder.
This effect can last for several months and the injections can be repeated if they help.
Although the symptoms of incontinence may improve after the injections, you may find it difficult to completely empty your bladder.
If this happens, you’ll need to be taught how to insert a thin, flexible tube called a catheter into your urethra to drain the urine from your bladder.
Botulinum toxin A is not currently licensed to treat urge incontinence or overactive bladder syndrome, so you should be made aware of any risks before deciding to have this treatment.
The long-term effects of this treatment are not yet known.
How Long Does Incontinence Last
One thing you should know is that most men regain continence following prostate surgery. If youre between the ages of 40 and 60, and generally healthy, the outlook is particularly good. In such cases, most men are no longer experiencing incontinence after about three months.
For others, it takes closer to a year. In such cases, there are effective treatments.
You May Like: Can Urinary Tract Infection Go Away Without Antibiotics
Urologic Symptoms Of Spinal Cord Disorders
Spinal cord lesions produce various types of voiding dysfunction, depending on the level of the neuraxis involved. Acute herniation of a central disk at L5-S1 is a neurosurgical emergency when the patient comes in with sudden onset of painful urinary retention. The nerve roots of the cauda equina that supply the detrusor travel medially. The sensory inputs from the bladder are not affected. In central herniation, patients usually experience no sciatic radiation of pain.
Spinal stenosis in the lumbosacral region, as it begins producing symptoms, usually results in intermittent episodes of urinary retention as a manifestation of intermittent claudication of the conus or cauda equina. Stenosis in the cervical region is more likely to produce long-tract involvement with bladder sphincter dyssynergia that is, contraction of the bladder is accompanied by abnormal contraction of the sphincteric mechanism.
Spinal cord injury above the sacral segments but below the pontine micturition center results, in the acute phase, in a state of so-called spinal shock. The detrusor is areflexic and insensate. Sphincteric activity continues. The patient may retain a large volume of urine. An indwelling catheter is usually placed to avoid overdistention, which in itself can render the bladder unresponsive.
What Questions Should I Ask My Healthcare Provider About Cauda Equina Syndrome
- What type of cauda equina syndrome do I have?
- What classification of cauda equina syndrome do I have?
- How quickly do I need surgery?
- How long will the surgery take?
- How long will I be in the hospital after surgery?
- Do I have a herniated disk?
A note from Cleveland Clinic
Cauda equina syndrome affects about 1 out of 65,000 people. Its uncommon, but its important to pay attention to the red flag symptoms because they might indicate various health issues. Be on the lookout for numbness in your saddle area, pain in your back and legs, problems with peeing or pooping, difficulties with sex and weakness in your extremities. See a healthcare provider immediately if you have these symptoms.
Learning that something is compressing the nerves in your back would frighten anyone. But don’t hesitate to go to the emergency department if you experience symptoms. The faster you get treatment, the less likely youll have permanent damage to your body, including incontinence and paralysis.
Last reviewed by a Cleveland Clinic medical professional on 11/22/2021.
References
Also Check: Amoxicillin 500mg For Urinary Tract Infection
How Can Physiotherapy Help My Urinary Incontinence Or Pain After Prostatectomy Surgery
Physiotherapy will focus on the strength, length, endurance and coordination of the pelvic floor muscles to help meet the new demands placed on the muscles after surgery.
It will also be important to examine and assess the pelvic and postural alignment that may be playing a role in incontinence or pain.
Lastly, it will be important to review and address concerns around constipation and/or voiding post-operatively to decrease the pressure on the pelvic floor.
How Long Does Urinary Incontinence After Prostate Surgery Last
The survival rate for prostate cancer is steadily improving, with the current 10-year survival rate is 98%. This is in large part due to better early detection, but also may be due to better surgical intervention. However, about 6-8% of men who have prostate surgery experience urinary incontinence, or leakage, after surgery.
Dr. Paul H. Chung is an experienced specialist with a deep understanding of male urinary incontinence. He can help you understand why youre having this uncomfortable problem, as well as suggest effective treatment strategies so that you dont have to continue to live with it.
Don’t Miss: What Is The Fastest Home Remedy For Urinary Tract Infection
How Common Is It
Most men thatâve had surgery to treat their prostate cancer experience some level of urinary problems. The challenges may be different for each man, but most issues are treatable and get better over time.
Recovery times, and how long you may need a pad will be different for each man. From 10 to 60% of men may still require a pad to control leaks 12 months after surgery.
Make sure to talk to your doctor or care team as theyâll know whatâs normal and where you may need help to manage your symptoms.
Posterior Tibial Nerve Stimulation
Your posterior tibial nerve runs down your leg to your ankle. It contains nerve fibres that start from the same place as nerves that run to your bladder and pelvic floor.
It’s thought that stimulating the tibial nerve will affect these other nerves and help control the urge to pee.
A very thin needle is inserted through the skin of your ankle and a mild electric current is sent through it, causing a tingling feeling and your foot to move.
You may need 12 sessions of stimulation, each lasting around 30 minutes, 1 week apart.
Some studies have shown that this treatment can offer relief from urge incontinence and overactive bladder syndrome for some people, although there’s not enough evidence yet to recommend tibial nerve stimulation as a routine treatment.
Tibial nerve stimulation is only recommended in a few cases where urge incontinence has not improved with medicine and you do not want to have botulinum toxin A injections or sacral nerve stimulation.
Read Also: Is Pineapple Good For Urinary Tract Infection
What Causes Loss Of Bladder Control After Spinal Cord Injury
The spinal cord transmits messages between the brain and body. However, after a spinal cord injury, messages may not be able to get past the site of injury, resulting in paralysis and loss of sensation below your level of injury.
Many people lose control of bladder functions after a spinal cord injury because the bladder muscles are innervated by some of the lowest nerve segments of the spinal cord. Damage to the spinal cord not only affects functions at the injury site but can also affect all functions below.
The reason why some spinal cord injury patients have normal bladder functions is because they have incomplete SCIs, which means some connections were not damaged by the injury. As a result, they may have some preserved motor control and sensation below their level of injury.
Next, well discuss different types of neurogenic bladder dysfunction that can result from spinal cord injury.