Specialized Tests To Diagnose Incontinence
Urology Specialists
Sometimes routine testing does not reveal the underlying cause, and further evaluation is required. You may be referred to a urologist or a urogynecologist for more specialized testing if your health concern is accompanied by pain, recurrent UTIs, blood or protein in the urine, neurological symptoms or muscle weakness, or pelvic organ prolapse. Women with this issue who have a history of radiation or surgery to the pelvic region may also be referred to a urologist.
Urodynamic Testing
Specialized testing can assess how well the bladder, urethra, and sphincters store and dispose of urine. There are many different types of instruments that can be used for urodynamic testing. Cystometry is a test that is used to help diagnose urge incontinence. It measures bladder pressure. The structures in the pelvis can be visualized with ultrasound. Uroflowometry can measure the volume of urine and flow rate. This test is used to determine the strength of related muscles and helps assess whether urine flow is blocked. There are other tests a urologist may perform depending on your symptoms.
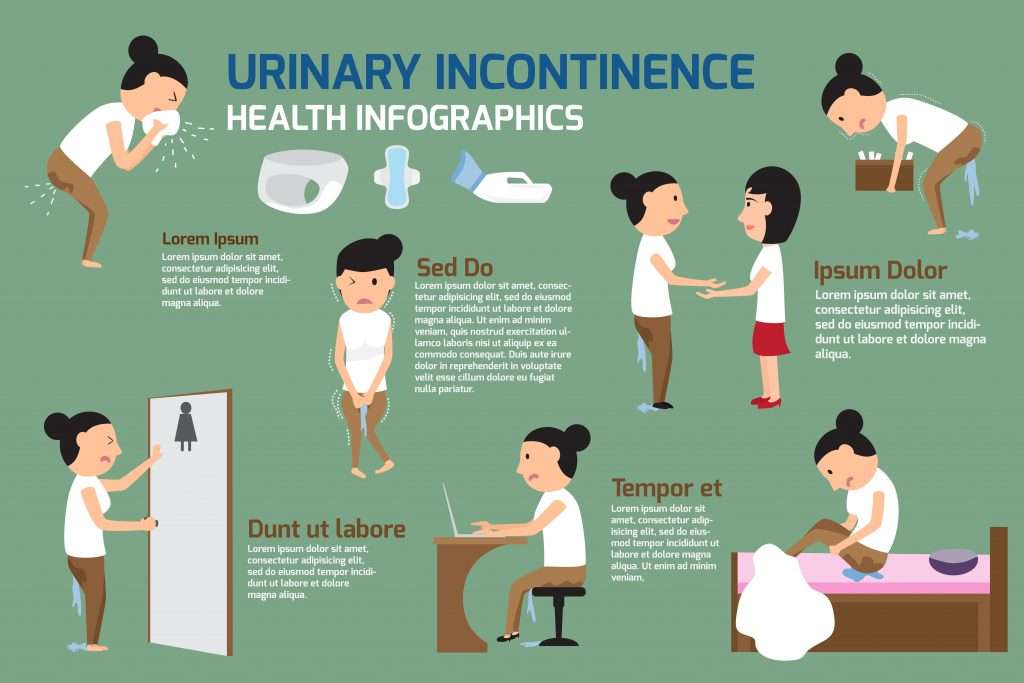
Urinary Incontinence In Women: Causes And Treatment
Urinary incontinence is twice as common in women than in men, and its especially common in older women. Among women ages 65 and older, 4 in 10 experience some loss of bladder control.The three main types of urinary incontinence are:
- Stress urinary incontinence, when you experience leakage or loss of urine when you laugh, sneeze, run or make some other sudden movement
- Urge incontinence, when you have a frequent or sudden urge to urinate
- Mixed, in which women experience symptoms of both types
When either form of urinary incontinence affects your quality of life, seek a medical professionals help. Beaufort Memorial has a team of womens health specialists trained in the latest treatments for this medical condition.
Request an appointment with an OB-GYN or gynecologist.
Urinary Incontinence And Underlying Conditions
Another main reason that women show signs of urinary incontinence is due to underlying conditions. As you get older, your organs start to age, and your muscles weaken. If youre healthy, however, this usually isnt the sole cause of incontinence. In many instances, incontinence is due to conditions like diabetes, poor heart function, or declining kidney health. Regardless of your age, its important to see your urologist regularly to make sure and understand whats causing problems to occur.
Recommended Reading: Physical Therapy For Urinary Problems
What Are Kegel Exercises
Kegel exercises, also called Kegels or pelvic floor muscle training, are exercises for your pelvic floor muscles to help prevent or reduce stress urinary incontinence. Your pelvic floor muscles support your uterus, bladder, small intestine, and rectum.
Four in 10 women improved their symptoms after trying Kegels.9 Kegels can be done daily and may be especially helpful during pregnancy. They can help prevent the weakening of pelvic floor muscles, which often happens during pregnancy and childbirth. Your pelvic floor muscles may also weaken with age and less physical activity.
Some women have urinary symptoms because the pelvic floor muscles are always tightened. In this situation, Kegel exercises will not help your urinary symptoms and may cause more problems. Talk to your doctor or nurse about your urinary symptoms before doing Kegel exercises.
A Urinary Incontinence Device To Prevent Bladder Leaks

In partnership with our friends at INNOVO
As a clinician and a researcher, Ruth Maher, DPT, PhD, has extensive experience with physical therapy for the pelvic floor to treat pain and incontinence and to support sexual health. One in three women experiences stress urinary incontinence , urine leaks caused by exertion or coughing. Exercises that strengthen the pelvic floor are an essential part of treatment however, Maher has found that many women are unable to contract the correct muscles. Often they are unaware that this is the case. Women would say they felt a contraction, but using ultrasound imaging, I could see that either there was no contraction of the pelvic floor muscles or other muscles, such as the glutes, were recruited, says Maher.
Maher saw the need for a therapy that could reliably stimulate contraction of the pelvic floor muscles to treat SUI, and she developed a prototype that delivered comfortable electrical stimulation through the skin rather than through the standard vaginal probe. This technology was the basis for INNOVO, a wearable device designed to quickly engage and strengthen pelvic floor muscles. INNOVO is FDA-cleared for the treatment of female stress urinary incontinence in the US. About womens reactions to the device, Maher says: They love it.
Read Also: What Can Cause Urinary Retention
Also Check: Why Do I Get So Many Urinary Tract Infections
What Is The Treatment For Urinary Incontinence
Specific treatment for urinary incontinence will be determined by your doctor based on:
-
Your age, overall health and medical history
-
Type of incontinence and extent of the disease
-
Your tolerance for specific medications, procedures or therapies
-
Expectations for the course of the disease
-
Your opinion or preference
Treatment may include:
-
Behavioral therapies:
-
Bladder training: Teaches people to resist the urge to void and gradually expand the intervals between voiding.
-
Toileting assistance: Uses routine or scheduled toileting, habit training schedules and prompted voiding to empty the bladder regularly to prevent leaking.
Diet modifications: Eliminating bladder irritants, such as caffeine, alcohol and citrus fruits.
Pelvic muscle rehabilitation :
Kegel exercises: Regular, daily exercising of pelvic muscles can improve, and even prevent, urinary incontinence.
Biofeedback: Used with Kegel exercises, biofeedback helps people gain awareness and control of their pelvic muscles.
Vaginal weight training: Small weights are held within the vagina by tightening the vaginal muscles.
Pelvic floor electrical stimulation: Mild electrical pulses stimulate muscle contractions.
Medication :
Pessary
Office procedure
Slings
Bladder suspension
Consult your doctor with questions regarding the management and treatment of urinary incontinence.
Sling Surgery Restores A Patient to Active Life | Stephanie’s Story
Fast Facts On Urinary Incontinence
- Urinary incontinence is more common in females than in males.
- There are a number of reasons why urinary incontinence can occur.
- Obesity and smoking are both risk factors for urinary incontinence.
Urinary incontinence is when a person cannot prevent urine from leaking out.
It can be due to stress factors, such as coughing, it can happen during and after pregnancy, and it is more common with conditions such as obesity.
The chances of it happening increase with age.
Bladder control and pelvic floor, or Kegel, exercises can help prevent or reduce it.
Treatment will depend on several factors, such as the type of incontinence, the patients age, general health, and their mental state.
You May Like: How To Use Tea Tree Oil For Urinary Tract Infection
Treatment Of Urinary Incontinence
Treatment for incontinence usually starts with the simplest treatments. This means trying lifestyle changes and other treatments before thinking about surgery. For information on things you can do to help yourself, see our section on self-help.
Treatment depends on the type of incontinence you have.
Oab Or Incontinence Medications Used In Canada
| Once daily |
| The most common adverse events found with anticholinergic medications include : dry mouth, constipation, impaired cognition and blurred vision. Talk to your doctor about limiting these side effects and which medication may be right for you. |
The two most commonly prescribed anticholinergic drugs are oxy- butynin and tolterodine , both of which are available in extended-release formulations.
Recently, medications have been developed that also limit unwanted side effects. These medications include darifenacin , solifenacin , trospium , fesotoredine , Myrbetriq® and oxybutynin chloride gel . Gelnique, is rubbed into the skin, making side effects like dry mouth milder because of constant absorption rates. Myrbetig is a new drug that works by a different mechanism to relax the bladder muscle without blocking the action of acetyl choline and therefore produces lesser side effects. The other drugs are anti-cholinergics but are more specific to the bladder muscle.
Neurotoxins
Re-injection can be considered when the effect diminishes but not within three months of the last injection
Estrogen
Since estrogen helps keep the urethra healthy and strong, the drop in estrogen that occurs in women after menopause especially with aging may contribute to incontinence. Applying estrogen in the form of a vaginal cream , tablet or ring may help ease symptoms of both stress and urge incontinence.
Desmopressin
Bulking agents
Read Also: Cystex Urinary Health Maintenance Reviews
C Data Abstraction And Data Management
Evaluations of the studies and data extraction will be performed independently by three researchers. The data abstraction forms are in Appendix 2. Errors in data extractions will be assessed by a comparison with the established ranges for each variable and the data charts with the original articles. Any discrepancies will be detected and discussed. We will abstract the information relevant to the PICOT framework for each question. We will abstract minimum datasets to reproduce the results that were presented by the authors. For categorical variables we will abstract a number of events among treatment groups to calculate rates, relative risk, and absolute risk differences . Means and standard deviations of continuous variables will be abstracted to calculate mean differences with a 95 percent confidence interval .
For randomized controlled trials , we will abstract the number randomized to each treatment group as the denominator to calculate estimates applying intention to treat principle. We will abstract the time when the outcomes were assessed as weeks from randomization and the time of followup post treatments. For observational studies we will extract crude rates or, preferably, relative measures of the association with standard error or 95 percent CI and reported adjustments for patient age, race, methods of detection, baseline variables, and comorbidities.
Urinary Incontinence In Older Adults
Urinary incontinence means a person leaks urine by accident. While it can happen to anyone, urinary incontinence, also known as overactive bladder, is more common in older people, especially women. Bladder control issues can be embarrassing and cause people to avoid their normal activities. But incontinence can often be stopped or controlled.
What happens in the body to cause bladder control problems? Located in the lower abdomen, the bladder is a hollow organ that is part of the urinary system, which also includes the kidneys, ureters, and urethra. During urination, muscles in the bladder tighten to move urine into the tube-shaped urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder dont work the way they should, urine can leak, resulting in urinary incontinence.
Incontinence can happen for many reasons, including urinary tract infections, vaginal infection or irritation, or constipation. Some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
Most incontinence in men is related to the prostate gland. Male incontinence may be caused by:
- Prostatitis, a painful inflammation of the prostate gland
- Injury or damage to nerves or muscles from surgery
- An enlarged prostate gland, which can lead to benign prostate hyperplasia, a condition in which the prostate grows as men age
Recommended Reading: Azo Urinary Tract Defense Vs Urinary Pain Relief
What Increases Your Risk
Sometimes several things combine to cause urinary incontinence. For example, a woman may have had multiple childbirths, be older, and have a severe cough because of chronic bronchitis or smoking. All of these might contribute to her incontinence problem.
Physical conditions that make urinary incontinence more likely include:
- Pregnancy and vaginal delivery.
Medicines and foods that may make urinary incontinence worse include:
- Caffeinated and carbonated drinks, such as coffee, tea, and soda pop.
- Alcohol drinks.
- Prescription medicines that increase urine production or relax the bladder .
- Smoking.
Dont Miss: What Causes Urinary Urgency And Frequency
Medications For Overactive Bladder
Drugs used to treat OAB block the abnormal contractions of the bladder muscle and can therefore also help ease the symptoms of urge urinary incontinence in both men and women. Youll find a list of OAB medications available in Canada on page 20. Generally speaking, these drugs fall into three categories:
Anticholinergics
Anticholinergic medications block the action of acetylcholine, a chemical messenger that tells the muscles of the bladder wall to contract. Unfortunately, acetylcholine acts in other parts of the body as well, so medications that block it can cause unwanted side effects like dry mouth, blurred vision, impaired cognition and constipation. New extended or prolonged release versions of anticholinergic medications reduce the incidence of side effects and improve compliance because they only need to be taken once a day to produce a steady absorption rate and constant blood levels of the drug.
Read Also: Urinary Tract Infection Leg Pain
A Criteria For Inclusion/exclusion Of Studies
The EPC will follow the Methods Guide for Comparative Effectiveness Reviews to select evidence from controlled trials and observational studies.85 Three investigators will independently decide on the eligibility of the studies according to recommendations from the Cochrane manual for systematic reviews.86 The algorithm to define eligibility of the studies will be developed for each research question .
Inclusion Criteria:
For question 1, we also plan to include the studies that evaluated different methods to diagnose UI in women in primary care settings and provide the number of true and false positive, true and false negatives, sensitivity, specificity, or predictive value of the diagnostic tests. We will apply criteria for assessing whether a body of trial data is sufficient to answer the question of diagnostic methods.85 We may include any observational studies that reported sensitivity and specificity of diagnostic methods for different types of female UI.
Exclusion Criteria:
S In Analysis To Handle Protocol Non
The primary analyses will be based on the observed data and a sensitivity analysis will be conducted where missing data are imputed using appropriate methods based on patterns of missingness. Data will be entered promptly, and data validation and cleaning will be carried out throughout the trial. Where spurious data are observed, values will be checked against available records.
You May Like: Artificial Sphincter For Urinary Incontinence
Availability Of Data And Materials
The Data Manager will manage access rights to the data set. Prospective new users must demonstrate compliance with legal, data protection and ethical guidelines before any data are released. Anonymous research data, including QRI audio-recordings and associated data, will be stored securely on research data storage facility and kept for future analysis with participant consent. We anticipate that anonymised trial data will be shared with other researchers to enable international prospective meta-analyses. Requests for access to data must be via a written confidentiality and DSA available from the RDSF website which will be confirmed by the CI . The DSA should cover limitations of use, transfer to third parties, data storage and acknowledgements. The person applying for use of the data will be scrutinised for appropriate eligibility by members of the research team.
Follow Directions To Manage Safety Concerns
Like any item worn in the vagina, bladder supports come with a small but important risk of toxic shock syndrome .
They can typically be worn safely for up to eight hours within a 24-hour period.
As with any other tampon or device youd insert into the vagina, youd want to make sure that its removed as directed, says Dr. Vasavada.
Don’t Miss: Hollister Vented Urinary Leg Bag
Recruitment Studyquintet Recruitment Intervention
The PURSUIT trial will employ an integrated QuinteT Recruitment Intervention aimed at optimising recruitment and informed consent . Recruitment challenges may arise in relation to identifying potentially eligible women, differences in levels of equipoise amongst clinicians and womens preferences for surgery or endoscopy. There may also be organisational challenges in relation to how the treatments are operationalised within the trial context and with the integration of the trial into existing clinical practice across sites. The QRI is aimed at identifying and addressing such recruitment difficulties promptly . In PURSUIT, the QRI will be carried out intensively in the internal pilot phase with lessons learnt used to sustain recruitment during the transition to the main trial phase, similar to other surgical trials where this has been successfully implemented .
The QRI uses novel qualitative and mixed-method approaches pioneered during the NIHR HTA-funded ProtecT study, later refined and applied to several other Randomised Control Trials , leading to insights about recruitment issues and the development of recruitment strategies . The QRI will proceed in two iterative phases.
A Good Alternative To Surgery
Bladder supports are often a good alternative to surgery. Theyre relatively comfortable and non-invasive, and you can wear them only when you need them.
A number of more active patients may use bladder supports because they just need something that will help when theyre being more physically active, says urologist Sandip Vasavada, MD.
Dr. Ferrando says theyre also a good option for women who simply want to avoid the possible risks or complications of surgery. So theyre not looking for surgery, they just want to manage it when theyre active, she says.
Read Also: Can You Get Urinary Tract Infection From Sex
Recommended Reading: Urinary Tract Infection After Period
Treatment For Urinary Incontinence In Women
Luckily, there are a number of different treatment options for urinary incontinence in women. Some of the treatment options include lifestyle changes while more serious cases might call for surgery, but each person is different. To better understand whats going on in your body, your urologist will need to first get a proper diagnosis.
Following your diagnosis, you will work with your urologist to create a treatment plan thats tailored to your needs. Most often, your doctor will recommend starting first with lifestyle changes to try and manage your symptoms. Some of these changes include performing kegel exercises regularly, maintaining a healthy weight, quitting smoking, and cutting out caffeine or alcoholboth of which are bladder irritants. During this time, you will also learn how to train your bladder and your doctor will recommend cutting back on liquids prior to going to bed. If you want to avoid any accidents during this time, consider looking into protective underwear or womens urinary incontinence products that can help catch any leaks.
In addition to Kegels, there are additional pelvic muscle rehabilitation techniques that your doctor might recommend. Biofeedback can help you perfect your Kegels and then you can move on to vaginal weight training to take things a step further. Some doctors may also discuss pelvic floor electrical stimulation with you as an option.