Tips For Managing Fecal Incontinence
Some of the most common strategies used to manage fecal incontinence include:
-
Bowel training: Similar to bladder training, bowel training encourages frequent visits to the bathroom, usually after meals. By having a bowel movement at the same time each day, its possible to prevent involuntary voids.
-
Medication: There are a number of drugs used to treat fecal incontinence. Some tighten the anal sphincter to prevent unwanted leakage, while others help loosen the stool, making it easier to pass.
-
Dietary changes. The foods a person consumes directly affect their bowel habits. Fruits and vegetables that are high in fiber minimize constipation by softening the stool. Fiber can also prevent diarrhea by absorbing water, making the stool bulkier.
What Incontinence Items Should I Include In A Stroke Recovery Kit
At Carewell, we carry many products that can assist with incontinence after a stroke. Heres a closer look at three of our most popular offerings:
Many stroke survivors wear or pull-ups in the initial stages of recovery. Prevail Total Care Underpads provide an additional layer of protection, preventing overflow leaks from soiling clothing, bedding, or furniture.
Key Benefits & Features:
-
Plastic backing to prevent leaks from soaking through
-
No clean-up required simply toss it in the trash can
-
Each underpad has an absorbent core that locks moisture in
A bathroom environment presents unique challenges to stroke victims. The small space and slippery surfaces may increase the risk of an accident like a slip-and-fall. McKessons commode chair with fixed arm can provide peace of mind. It has a folding-steel frame that allows for easy transport as well as plastic armrests that provide comfort and support.
Key Benefits & Features:
-
Supports up to 350 pounds of weight
-
Includes a 7.5-quart commode bucket with handle for easy disposal
-
Non-skid tips for improved safety
-
Hassle-free assembly
What if I have questions regarding incontinence products?
Caring for a stroke survivor with urinary or bowel dysfunction presents unique challenges. Our friendly and compassionate Care Team will be happy to assist you in finding the products that best align with your needs. To get in touch, call 855-1666 or email .
Incontinence Is Usually Temporary And Always Manageable
Thankfully, long-term incontinence is uncommon following a stroke and the latest research suggests that only about 15 percent of stroke patients will continue to experience incontinence issues one year after suffering a stroke. Nonetheless, even short-term incontinence can be upsetting and embarrassing for survivors. Here at Saebo, we are committed to stroke support and recovery for all survivors and their families. Saebo offers a wide range of products that combine cutting-edge technology with evidence-based rehabilitation techniques. Our offerings and network of Saebo-trained therapists can help you or a loved one to obtain all the necessary tools to maximize stroke recovery.
All content provided on this blog is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately. Reliance on any information provided by the Saebo website is solely at your own risk.
Also Check: Healing Urinary Tract Infection Without Antibiotics
First Some Fast Facts
There are two types of strokes, ischemic stroke, and hemorrhagic stroke.
The ischemic stroke is the more common one, and it occurs when a blood clot blocks a blood vessel in the brain, causing brain cells to quickly die from the lack of blood circulation and oxygen, which in turn causes the body to lose some neurological functions. The ischemic stroke can also occur when plaque builds up inside an artery, causing it to narrow and eventually become blocked.
If you have suffered a mini ischemic stroke , you are at risk of suffering a more serious one.
Hemorrhagic stroke is the second type, and it happens when the blood vessel bursts or leaks.
In the United States, stroke is the fifth leading cause of adult death and disability, and nearly 800,000 people experience strokes each year.
These conditions can make you more at risk of stroke: diabetes, heart disease, obesity, and high cholesterol level.
If You Suffer From Urinary Retentioncheck Out Compactcath
We produce catheters that are compact, mess-free, non-touch, and pre-lubricated. They are discreetly designed, convenient, and perfect for those who lead an active life.
CompactCath® is designed at Stanford d.school. It is FDA-cleared in 2014, holds six patents, covered by CNN Money, won two grants and two iF product design awards .
Read Also: How To Prevent Urinary Retention
Transcutaneous Electrical Nerve Stimulation
The use of TENS therapy to treat urge incontinence in the non-stroke population has a growing body of evidence to support it.18,19 There have, however, only been two small RCTs that have reported on its use in stroke survivors.21,22 Guo et al. randomised 61 participants to 30 minutes of TENS therapy at 75Hz once daily for 60 days or usual therapy. The results demonstrated a positive impact in favour of the treatment arm in all three primary outcomes of improved pre-/post-overactive bladder symptom score, Barthel Index of activities of daily living score and urodynamic values.
The statistically significant results also suggested improved bladder capacity for those in the treatment arm.21 The second RCT in 81 participants aimed to study what effects TENS therapy at two different frequencies had on post-stroke UI.22 A group receiving basic rehabilitation and no TENS therapy was used as a control. The study protocol maintained that both treatment arms received 30 minutes of TENS therapy a day for 90 days at their respective frequencies. Primary outcomes were identified as pre-/post-overactive bladder symptom scores, Barthel Index of ADL scores and urodynamic values as well as the number of UI episodes within a 24-hour period. The results again demonstrated statistically significant improvements in all primary outcomes in favour of both treatment arms when compared with control.
You May Like: What Is The Antibiotic For Urinary Tract Infection
What Is Incontinence After Stroke
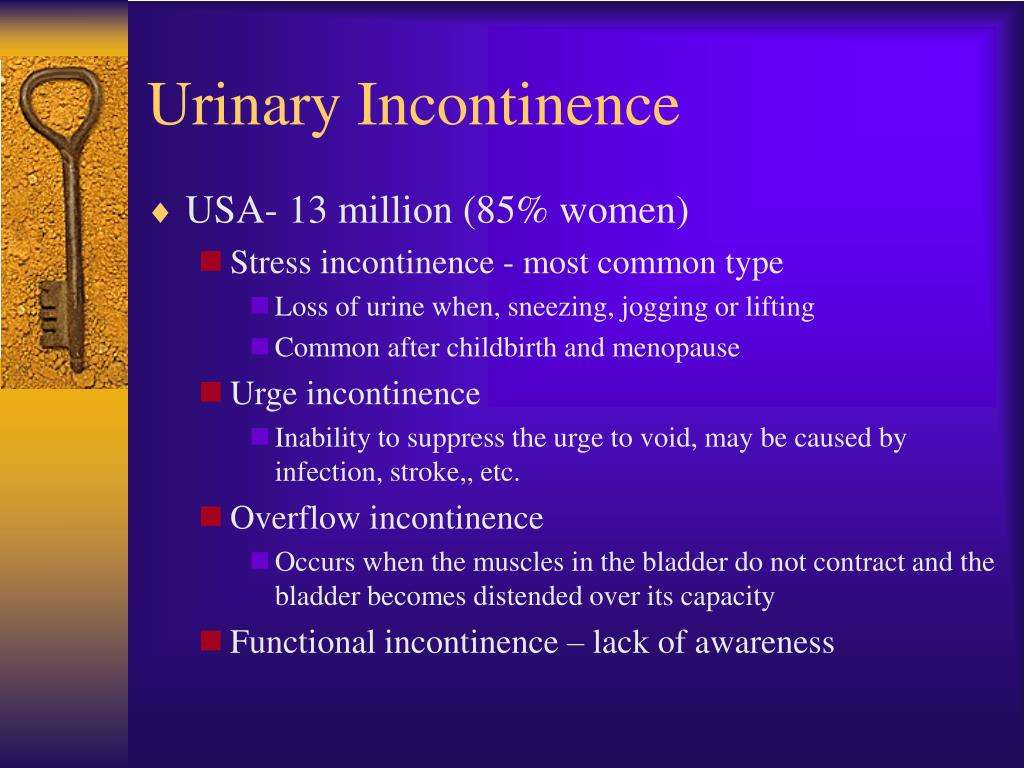
Incontinence is the involuntary loss of urine from the bladder or feces or wind from the bowel, according to the Continence Foundation.
There are varying degrees of incontinence. Some may experience light leaking while others may have a complete loss of bowel and bladder control.
Incontinence after stroke occurs when a stroke affects the area of the brain that controls your bladder and bowels. Studies often suggest that damage to the frontal lobe results in bladder dysfunction after stroke. However, some studies suggest that damage to other areas of the brain such as the brainstem, temporal lobes, internal capsule, frontal cortex, or frontoparietal lobes also affect bladder control.
Factors that place individuals at an increased risk of incontinence after stroke include:
- High severity of stroke
- Hypertension
- Comorbidity of other disabling diseases
In this study of 935 acute stroke patients, 47% of individuals had urinary incontinence upon admission. However, in a 6-month follow-up, only 19% reported urinary incontinence. Likewise, 40% had fecal incontinence upon admission while only 9% had it by the 6-month follow-up.
This demonstrates that incontinence after stroke can be treated and individuals may be able to regain bowel and bladder control.
In the following section, well share some helpful tips for managing incontinence after stroke.
Also Check: What Antibiotics Are Best For Urinary Tract Infections
Treatments For Bowel Problems
Advice and treatment for bowel problems may include:
-
Bowel retraining involves regular visits to the toilet. This is usually after meals, when the bowels are stimulated to move by a natural reflex. You also learn to delay bowel movements once on the toilet to improve your ability to hold on.
-
Pelvic floor exercises can strengthen the muscles that control bowel movement.
-
Dietary changes such as eating more fibre.
-
Medication: mainly laxatives to treat chronic constipation and impacted stool, which is the most common cause of leaking faeces. If you have true diarrhoea, medication can help. It is important you seek help to find out what is causing your bowel problem.
-
Drinking more fluids helps soften the stools.
-
Enema or bowel irrigation may be used to clear the bowel if faecal impaction occurs.
Other Things You Can Do
A dietitian can help you get the right balance of fibre and fluid in your diet. If you increase the fibre in your diet you may need to increase the fluid you drink too.
Drink up to eight to ten cups of fluid a day. Water is best. This can help stop bladder irritation and make it easier to pass faeces. Try to reduce your intake of drinks that make you need to go to the toilet more often. This includes drinks with caffeine such as tea and coffee.
Set up your toilet and bathroom so you can get in quickly and safely. Wear clothing that can be undone quickly.
Before you leave hospital make sure:
- You know how to manage your incontinence.
- You can access any continence aids you may need.
- You know about follow up appointments you may have.
- Your family know about your difficulties and the plan to manage them.
Read Also: Tea For Urinary Tract Health
You May Like: Urinary Tract Infection Blood Clots
Improving The Ability To Do Ways To Deal With Post
This action needs to be done in management of post-stroke UI. The results of our qualitative study showed that the informants/patients did several ways to overcome their post-stroke UI such as bladder retraining, pelvic floor muscle exercises, distraction technique, and ROM exercises. These ways describe the knowledge, skills, and ability to decide what the patient should do in dealing with his illness. Based on these findings, it appears that the patient is not only focused on improving the functional ability to urinate but also improving the functional ability to walk. In dealing with post-stroke UI, patients need to be trained to improve the functional ability to urinate as well as the functional ability to walk .
Continental training begins as soon as the patients condition stabilizes. It is also important to prevent incontinence which may be reversible . Bladder retraining requires that patients be independent and motivated to actively participate in treatment . Bladder retraining trains the patient to empty the bladder at regular intervals. Emptying the bladder at regular time intervals in post-stroke UI patients is a more effective method for treating incontinence .
Help For Bowel Problems
Try these strategies:
Watch your diet. Be sure to drink enough liquid during the day. Eat high-fiber foods like vegetables, fruits, beans, and whole grains.
Stay active. When you move your body, it helps keep things moving in your colon, too.
Bowel retraining. Try to poop at the same time each day. But be careful not to strain.
Medications. Ask your doctor if any medicines youâre taking cause constipation. There might be others you can try instead.
You can try a stool softener or a laxative to ease constipation. If it doesnât get better, ask your doctor if you should try other ways to get things moving, such as an enema — liquid that goes in your bottom to clear out your colon — or a type of suppository called a bulking agent.
If you have trouble with leaks, there are medicines that slow down the waste in your colon and make it firmer.
Read Also: Over The Counter Products For Urinary Tract Infections
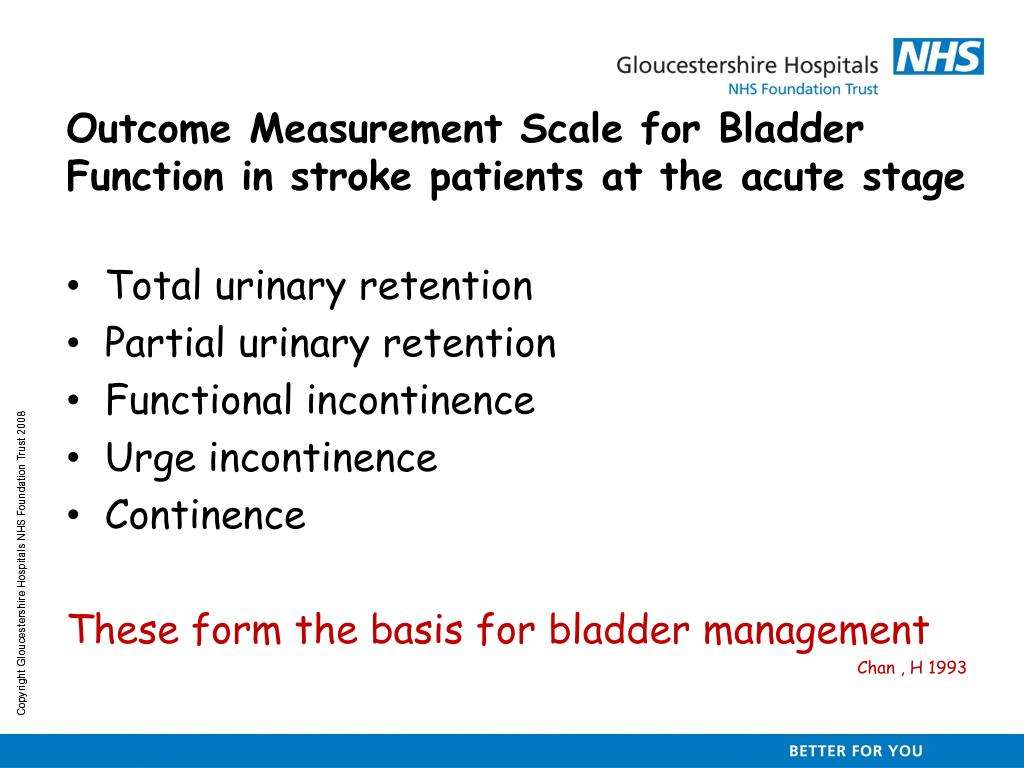
Current Policy And Evidence To Guide The Management Of Post
The importance of effective continence management is recognised within national stroke guidelines14 that recommend:
- Ensuring staff are trained in the use of a standardised assessment and management protocol for post-stroke UI.
- Treating the identified cause of incontinence and reassessing/designing a treatment plan that may include referral to specialist continence services and/or supplying adequate supplies of continence aids for patients who remain incontinent two weeks after onset.
- Training the person affected by the stroke and/or their carers in the management of UI.
- Offering behavioural interventions such as prompted/timed voiding, bladder retraining, PFMT, and where appropriate external equipment.
Potential Biases In The Review Process
The original protocol for this review specified inclusion criteria for participants as having had a stroke in the previous 12 months, but this definition proved unworkable, because most of the trials did not specify or report time since stroke. There was also a lack of clarity about whether urinary incontinence was subsequent to stroke. Only three trials specified that urinary continence problems were subsequent to stroke, and detailed the time since stroke onset. For this reason, the extent to which the results for the remaining trials can be generalised to people with continence problems solely as the result of a stroke is unclear.
Read Also: Home Remedies For Urinary Tract Infection In Females
Ethical Approval And Trial Registration
This study was performed according to the ethical guidelines of the Declaration of Helsinki and approved by the Eastern Switzerland Ethics Committee responsible for the same. All participants or their representatives provided oral and written informed consent. The study was registered in the German Clinical Trials Register .
Read Also: Urinary Tract Infection After Period
Exercises To Improve Continence
An effective way to regain control over your bowel and bladder muscles after stroke is to practice targeted exercises.
Whenever you repeatedly practice something, it activates neuroplasticity and rewires the brain. Neuroplasticity is how the brain heals itself after stroke, including healing the secondary effects of stroke like incontinence.
So if you want to improve incontinence long-term, try these exercises that can help treat incontinence.
- Bladder/bowel training involves gradually retraining your bladder and bowels to hold more for longer. Start by setting specific times to go to the restroom, and then each week increase the amount of time between each bathroom break. However, dont wait more than a few hours between bathroom breaks if possible.
- Pelvic floor training can help you strengthen the muscles that support your bladder, small intestine, and rectum. To do this exercise, squeeze the muscles that you use to stop urinating for 3 seconds, then relax for 10-20 seconds. Continue this for 10 reps while adding one second to each repetition.
These exercises will help increase the length of time between bathroom breaks and strengthen the muscles that control continence.
The more you practice the skill of controlling your bladder/bowel movements, the better you will get at it.
Don’t Miss: What Is The Best Medicine For Urinary Tract Infection
Can Incontinence After A Stroke Be Cured
Incontinence after stroke can absolutely be cured, but it will take time and most incontinence symptoms can be improved. Again, remember everyone heals differently from a stroke and the hope is to get the individual back to as close as they were functioning prior to the stroke, and this includes bladder function. For example, if the individual was struggling with urinary urgency prior to the stroke, it could worsen or take longer to improve post-stroke. While recovering from a stroke and dealing with incontinence symptoms, individuals, or their loved ones, can supplement their treatment with continence products such as bladder control pads and protective underwear.
Overall Completeness And Applicability Of The Evidence
The major point of interest in the included studies is the mix of categories of intervention, including physical, behavioural and complementary therapies, drugs, and professional input interventions such as using trained personnel and specific methods of managing care. However, within categories it was generally not possible to combine studies due to use of different outcome measures.
Read Also: What Can Cause A Urinary Tract Infection In Males
Exercises In Bladder And Bowel Control
These are common techniques and exercises for bladder and bowel retraining:
- Timed voiding. Also known as prompted voiding, it involves scheduling bathroom breaks at specific times to avoid the sudden and uncontrollable need to go. The goal is to increase the length of time between scheduled bathroom breaks.
- Urgency control. A combination of deep breathing and complex mental tasks help ignore the need to go. One example of a complex mental task is counting down from 100.
- Pelvic floor muscle training. Also known as Kegel exercises, builds strength in the pelvic floor muscles leading to better muscle and bladder control.
- Medication. Stool softeners or laxatives can help with bowel incontinence and other medications can help with urinary incontinence.
Improving The Provision Of Information And Understanding Of Post
The basis for implementing this theme is the finding of our previous qualitative study which showed that informants need information to increase their knowledge in recognizing and understanding various physical and psychosocial conditions that occur to them. This information can make it easier for patients to overcome problems related to post-stroke UI that they were experiencing.
Information is provided through health education about post-stroke UI which includes an explanation of the basic concepts of post-stroke UI such as definition, causes, the process of occurrence, signs and symptoms that appear, types of post-stroke UI, and how to deal with post-stroke UI. Nurses need to build a trusting relationship and conduct an initial assessment of the patients knowledge regarding the patients perceived physical and psychosocial conditions.
Read Also: Does Cranberry Juice Clean Urinary Tract
Treatments For Bladder Problems
Once the cause of your bladder problem has been found, you will be offered advice and treatment. These can include:
-
Drinking plenty of fluids. Strong, concentrated urine irritates your bladder. This makes feelings of urgency worse, can cause leakage and also bladder infections. Caffeine can also stimulate urine production so you may be advised to reduce your caffeine intake.
-
Bladder training reduces urgency and frequency by gradually teaching your bladder to hold more urine. This is done by making regular visits to the toilet, and gradually extending the time between visits until your bladder learns how to hold on.
-
Pelvic floor exercises help strengthen muscles so that they provide support. This will help improve bladder control and improve or stop leakage of urine.
-
Electrical stimulation devices, which can be inserted in either the vagina or the anus to stimulate and strengthen the muscles that control the bladder.
-
Using medication to reduce feelings of urgency and frequency, or reduce the amount of urine your body makes.
-
Weight loss often improves bladder control in the longer term.
-
Stopping smoking: coughing makes bladder leakage worse. Stopping smoking can help.