Enuresis Not Due To A Substance Or Known Physiological Condition
- 2016201720182019202020212022Billable/Specific Code
- 2016201720182019202020212022Billable/Specific Code
Code Also
- 2016201720182019202020212022Non-Billable/Non-Specific Code
- any associated overactive bladder
- urinary incontinence associated with cognitive impairment
- urinary incontinence NOS
- 2016201720182019202020212022Billable/Specific Code
Applicable To
- stress incontinence and other specified urinary incontinence
- urinary incontinence NOS
- Applicable To annotations, or
What Kinds Of Surgeries Treat Urinary Incontinence After Your Prostate Is Removed
There are two types of surgery for urinary incontinence: the urethral sling and the artificial urinary sphincter. Usually, the incontinence needs to last for about one year after the prostatectomy to be sure there is not going to be further improvement before your healthcare provider suggests this type of therapy.
What Is An Artificial Urinary Sphincter And How Does It Help With Urinary Incontinence
An artificial urinary sphincter can help men who have moderate to severe urinary incontinence due to poorly functioning muscle or sphincter valve after prostate cancer surgery.
The AUS has three parts:
- An inflatable cuff that is placed around the upper urethra. The cuff closes off the urethra to prevent leakage of urine.
- A pump that is inserted into the scrotum. It’s completely on the inside and not visible, and the pump controls the opening and closing of the cuff.
- A small pressure-regulating balloon that is placed in the abdomen, under the muscles. The balloon maintains fluid under pressure within the urethral cuff to pressurize the system and hold urine back.
If you have this surgery, youll press on the pump when you feel the need to pee. This opens the cuff to allow urine to pass. When youre done peeing, the cuff automatically closes again on its own.
The AUS procedure provides a very good and satisfactory result in 90% of cases. Risks are uncommon and include:
- Failure of the device .
- Erosion of the cuff into the urethra.
- Infection.
All of these would require additional surgery.
You May Like: Urinary Tract Infection Azo Cranberry
Drg Mapping Rules For R3981
Diagnostic codes are the first step in the DRG mapping process.
The patient’s primary diagnostic code is the most important. Assuming the patient’s primary diagnostic code is R39.81, look in the list below to see which MDC’s “Assignment of Diagnosis Codes” is first. That is the MDC that the patient will be grouped into.
From there, check the subsections of the MDC listed. The patient will be mapped into the first subsection for which the treatment performed on the patient meet the listed requirements of that subsection.
DRG grouping rules are adjusted each year, so make sure to check the rules for the fiscal year of the patient’s discharge date.
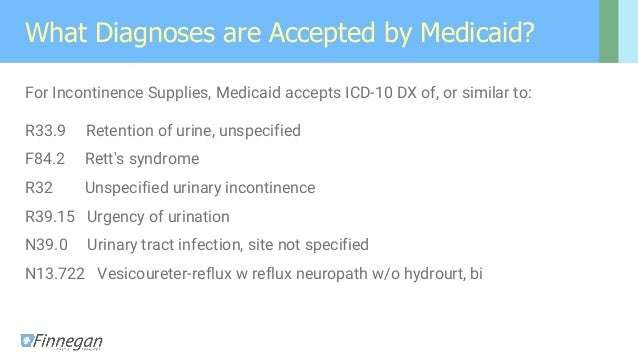
Retention Of Urine Unspecified
- 2016201720182019202020212022Billable/Specific Code
- R33.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM R33.9 became effective on October 1, 2021.
- This is the American ICD-10-CM version of R33.9 – other international versions of ICD-10 R33.9 may differ.
- Applicable To annotations, or
Read Also: Drugs To Control Urinary Incontinence
The 4 Types Of Urinary Incontinence And How They Are Diagnosed
If youve ever leaked urine or had trouble getting to the bathroom quickly enough, youre not alone. Almost half of all women leak urine at some point in their lives a condition known as urinary incontinence.
Urinary incontinence can be frustrating and embarrassing. Fortunately, treatment can make a difference. At Virtuosa GYN in San Antonio, Texas, Dr. Susan Crockett offers patients with urinary incontinence a full range of treatment options, from lifestyle changes and exercise to medication and surgery.
To give you a better understanding of your condition, Dr. Crockett offers the following information about the main types of urinary incontinence, along with details about what causes them and how they are diagnosed and treated.
What Is Urinary Incontinence And How Is It Related To Prostate Cancer Surgery
Urinary incontinence is the loss of the ability to control urination . Urinary incontinence sometimes occurs in men who’ve had surgery for prostate cancer.
If youve had prostate cancer surgery, you might experience stress incontinence, which means you might leak urine when you cough, sneeze or lift something that is heavy. This happens because of stress or pressure on the bladder. There is also a type of incontinence that is called urge incontinence. When this happens, you are hit with a sudden need to urinate right away and have leakage before you can make it to the bathroom.
Read Also: Urinary Incontinence In Child Treatment
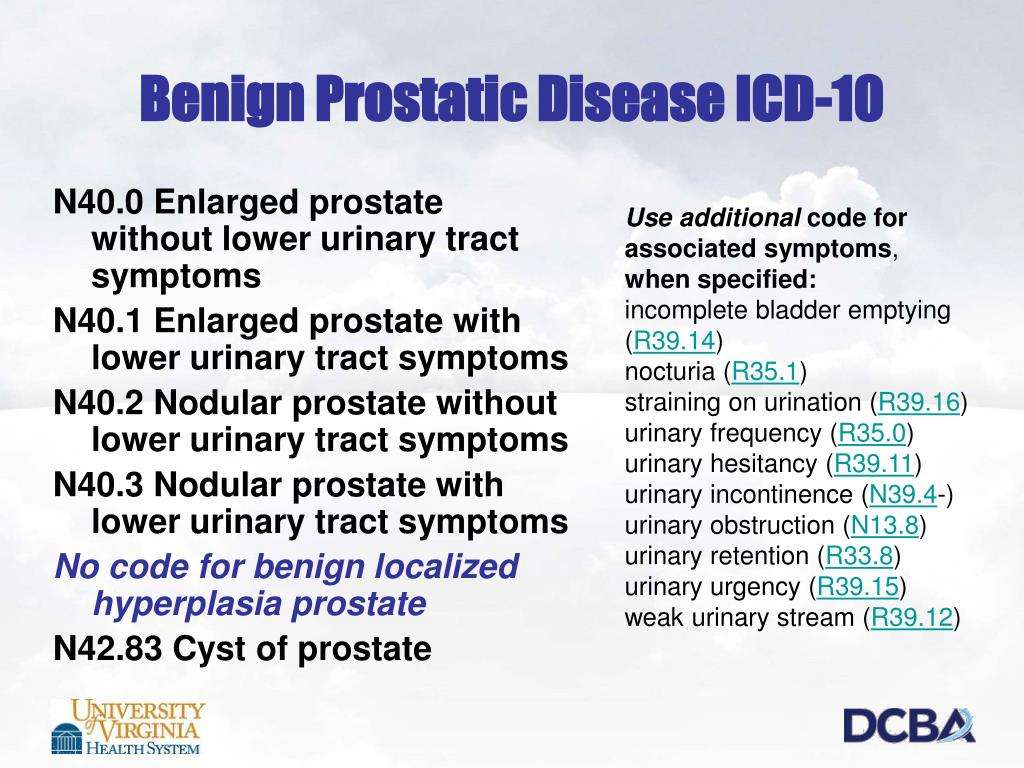
Determining The Correct Urinary Incontinence Icd 10 Code
Your patient just presented with urinary incontinence. Its been a while since youve had to recall the different types of urinary incontinence, not to mention the treatment options, device reimbursement qualifications, and urinary incontinence ICD 10 coding. Heres a quick refresher of the most common types of incontinence:
- Stress urinary incontinence is an involuntary loss of urine with a sudden increase in abdominal pressure. These patients leak when they sneeze, laugh, cough, or exercise. It is the most common type of incontinence. It affects women more frequently than men, often starting after the trauma of childbirth.
- Urge urinary incontinence occurs when patients have a sudden urge to urinate and subsequent loss of bladder control. It is associated with detrusor muscle hyperactivity. Urge incontinence occurs in both men and women, with a higher incidence among the elderly.
- Mixed urinary incontinence presents with symptoms of both stress and urge incontinence. It is more common to have mixed incontinence than to have solely urge incontinence.
- Overactive bladder is basically urge incontinence without the leaks. These patients are quick enough and mobile enough to get to the toilet before having an accident.
Other types of incontinence include overflow incontinence, functional incontinence, and variations of fecal incontinence. Each type has its own urinary incontinence ICD 10 code.
What Happens After Urethral Sling Surgery
Patients usually recover from this surgery quickly. It’s best to limit demanding activities for approximately six weeks after surgery to avoid having the sling loosen before healing is complete.
After surgery, there may be swelling that makes it difficult to urinate. You’ll have a catheter coming out of the urethra for two to three days. After this, the catheter is removed and just about everyone is able to void on their own. In rare cases, the catheter may have to be reinserted for a few days or up to a week if you cannot urinate.
After the swelling goes down, youll gradually be able to urinate on your own and empty your bladder. However, your normal urination pattern may not return for a few weeks.
The majority of men who’ve had this procedure have been cured of their urinary incontinence and no longer use pads. The others usually improve to the point where they don’t use as many pads as they were before.
Read Also: Herbal Tea For Urinary Health
How Is Urinary Incontinence Diagnosed
Your health care provider may use many tools to make a diagnosis:
- A medical history, which includes asking about your symptoms. Your provider may ask you to keep a bladder diary for a few days before your appointment. The bladder diary includes how much and when you drink liquids, when and how much you urinate, and whether you leak urine.
- A physical exam, which can include a rectal exam. Women may also get a pelvic exam.
- Urine and/or blood tests
- Imaging tests
Who Is At Risk For Urinary Incontinence
In adults, you are at higher risk of developing UI if you
- Are female, especially after going through pregnancy, childbirth, and/or menopause
- Are older. As you age, your urinary tract muscles weaken, making it harder to hold in urine.
- Are a man with prostate problems
- Have certain health problems, such as diabetes, obesity, or long-lasting constipation
- Are a smoker
- Have a birth defect that affects the structure of your urinary tract
In children, bedwetting is more common in younger children, boys, and those whose parents wet the bed when they were children.
Read Also: Foods To Prevent Urinary Tract Infections
Disorder Of Urinary System Unspecified
- 2016201720182019202020212022Billable/Specific Code
- N39.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM N39.9 became effective on October 1, 2021.
- This is the American ICD-10-CM version of N39.9 – other international versions of ICD-10 N39.9 may differ.
- Applicable To annotations, or
Symptoms Signs And Abnormal Clinical And Laboratory Findings Not Elsewhere Classifiednote
Don’t Miss: Can A Urinary Tract Infection Cause An Elevated Psa
Did I Prescribe The Right Treatment
When youve diagnosed the patient and figured out the correct urinary incontinence ICD 10 code, its time to recommend an appropriate treatment. Primary care physicians and gynecologists may not be familiar with all the at-home options to treat their stress urinary incontinence patients. Typical suggestions include Kegel exercises and limiting fluid intake, and currently, there are no medications approved to treat stress urinary incontinence. Invasive treatments include surgery, internal tissue manipulation, and intravaginal monitoring and stimulation, plus these treatments typically require a specialists care.
For patients with mild to moderate incontinence symptoms, it may be preferential for the primary care physician or gynecologist to provide conservative care directly. This approach results in more immediate care for the patient, continuity of care to monitor progress, and minimized costs.
- Want to supplement or have limited access to pelvic floor physical therapy.
- Have trouble performing Kegel exercises correctly .
- Prefer the convenience and privacy of in-home treatment.
- Need care after their 6-week postpartum checkup.
What Are The Treatments For Urinary Incontinence
Treatment depends on the type and cause of your UI. You may need a combination of treatments. Your provider may first suggest self-care treatments, including
- Lifestyle changes to reduce leaks:
- Drinking the right amount of liquid at the right time
- Being physically active
- Staying at a healthy weigh
- Avoiding constipation
- Not smoking
If these treatments do not work, your provider may suggest other options such as
- Medicines, which can be used to
- Relax the bladder muscles, to help prevent bladder spasms
- Block nerve signals that cause urinary frequency and urgency
- In men, shrink the prostate and improve urine flow
Read Also: Can Allergies Cause Urinary Problems
Is Elitone Covered By Insurance
In addition to determining the correct urinary incontinence ICD 10 code, treatment devices correlate with certain codes. HCPCS code E0740 applies to non-implantable pelvic floor muscle stimulators, including ELITONE. Note that PDAC recently reviewed this code and found that many previously covered devices, specifically those that provide biofeedback but do not provide e-stim, do not fall within the scope of E0740 and are not covered. To fall within the category of the code, the device must deliver stimulation that exercises the pelvic floor muscles.
ELITONE received approval to utilize E0740 shortly after it received FDA clearance. Many private insurers cover ELITONE and have published coverage decisions . Although requirements vary, most insurers have two stipulations: a prescription and failed improvement with four weeks of pelvic floor exercises.
Unlike other e-stim devices, ELITONE is also available as an FDA-cleared, over-the-counter product and can be purchased by patients directly from the ELITONE website. This is an excellent solution for patients without insurance coverage or who want immediate access to treatment.
What Is A Urethral Sling Procedure And How Does It Help With Urinary Incontinence
In the urethral sling procedure, a synthetic mesh tape is placed around part of the urethra, moving the urethra into a new position. This is a minimally invasive procedure, which means that the surgeon only has to make a small incision in the perineum .
Your provider may recommend a urethral sling procedure if you have mild to moderate urinary incontinence after a radical prostatectomy that hasnt improved using other more conservative measures. It’s highly successful in helping men overcome incontinence, or reduce episodes of leaking urine.
Before the surgery, the provider may do some tests, including the following:
- A urodynamic study, to test how well the bladder is working.
- A 24-hour pad test .
- A cystoscopy, a test in which the doctor looks inside the bladder with an instrument called a cystoscope.
You dont have to donate any of your own blood before surgery.
You May Like: What Causes Frequent Urinary Tract Infections
R399 Unspecified Symptoms And Signs Involving The Genitourinary System
NEC Not elsewhere classifiableThis abbreviation in the Tabular List represents other specified. When a specific code is not available for a condition, the Tabular List includes an NEC entry under a code to identify the code as the other specified code.
NOS Not otherwise specifiedThis abbreviation is the equivalent of unspecified.
This note further define, or give examples of, the content of the code or category.
List of terms is included under some codes. These terms are the conditions for which that code is to be used.The terms may be synonyms of the code title, or, in the case of other specified codes, the terms are a list of the various conditions assigned to that code.The inclusion terms are not necessarily exhaustive. Additional terms found only in the may also be assigned to a code.
Certain conditions have both an underlying etiology and multiple body system manifestations due to the underlying etiology.For such conditions, the ICD-10-CM has a coding convention that requires the underlying condition be sequenced first, if applicable, followed by the manifestation.Wherever such a combination exists, there is a use additional code note at the etiology code, and a code first note at the manifestation code.These instructional notes indicate the proper sequencing order of the codes, etiology followed by manifestation.
What Is The Prostate’s Role In Urination
When urine is emptied into the bladder from the kidneys, it’s kept inside the body by a couple of valves that stay closed until your body tells them to open when you urinate.
If youve had your prostate completely removed, youve had a surgery called radical prostatectomy. Along with the prostate gland, the surgeon has to remove one of the valves outside the prostate that open and close to let urine out or keep it in. Usually having one working valve is enough, but there might also be also be some effect on the nerves and muscles in the area from the surgery that allows urine to leak. Approximately 6% to 8% of men who’ve had surgery to remove their prostates will develop urinary incontinence.
Also Check: Itching In Urinary Tract Male
How Is Urinary Incontinence After Prostate Surgery Treated
If you find youre having issues with mild to moderate leakage after surgery, your healthcare provider might suggest starting with noninvasive therapies like medications or physical therapy exercises for the pelvic floor muscles. These treatments may also cut down on the number of times that you have to get up each night to pee.
These methods can sometimes help men who have mild to moderate leakage. Men who have persistent leakage or a more severe problem may need surgery if they do not want to continue to use pads.
Coding Notes For R3981info For Medical Coders On How To Properly Use This Icd

- Inclusion Terms:
Inclusion Terms
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
- Urinary incontinence due to cognitive impairment, or severe physical disability or immobility
- Code Type-1 Excludes:
Type-1 Excludes
Type-1 Excludes mean the conditions excluded are mutually exclusive and should never be coded together. Excludes 1 means “do not code here.”
Read Also: Best Remedy For Urinary Tract Infection