Dysfunctional Breathing In Myasthenia Gravis
It has long been observed that breathing patterns and the central ventilator drive can be altered in patients with mild or moderate MG . In our practice, we have observed several patients, who we deem stable or in minimal manifestations, complaining of dyspnoea as a residual prominent symptom in spite of them not having any objective evidence of respiratory muscle weakness. A very small proportion, may have had a MG crisis at some stage of their disease, which inevitably raises long-term anxiety levels to the patient and their carer, about the potential severity and sometimes unpredictability of the disease. In some, contributory factors are clear and include deconditioning or weight gain. We have identified, through collaborative work with the local respiratory team, that many of these patients have developed dysfunctional breathing . Our local respiratory physiotherapist has been working with these patients, employing physiotherapy-based breathing pattern modification interventions. These include relaxation of intercostal muscles, accessory muscles and full utilization of the diaphragm thus helping them to regulate and improve their breathing pattern with good results .
Treatment Of Myasthenia Gravis
In plasma exchange Plateletpheresis In addition to normal blood donation and transfusion, special procedures are sometimes used. In plateletpheresis, a donor gives only platelets rather than whole blood. Whole blood is drawn from… read more , toxic substances are filtered from the blood. Improvement after plasma exchange is similar to that after taking immune globulin.
What Are The Symptoms Of Urinary Incontinence
The symptoms of urinary incontinence depend on the type of condition you have.
There are several types of urinary incontinence, but the most common are:
- stress incontinence when the pelvic floor muscles are too weak to prevent urination, causing urine to leak when your bladder is under pressure, for example when you cough or laugh
- urge incontinence when urine leaks as you feel an intense urge to pass urine, or soon afterwards
These two types of urinary incontinence are thought to be responsible for over 9 out of 10 cases. It is also possible to have a mixture of both stress and urge urinary incontinence.
Read more about the symptoms of urinary incontinence.
Recommended Reading: Urinary Tract Infection In Babies
Signs And Symptoms Of Multiple Sclerosis
Myasthenia gravis may occur gradually or suddenly. Signs and symptoms include:
- weak eye closure, ptosis, and diplopia from impaired neuromuscular transmission to the cranial nerves supplying the eye muscles .
- skeletal muscle weakness and fatigue, increasing through the day but decreasing with rest
- progressive muscle weakness and accompanying loss of function, depending on the muscle group affected, that becomes more intense during menses and after emotional stress,prolonged exposure to sunlight or cold, or infections
- blank and expressionless facial appearance and nasal vocal tones secondary to impaired transmission of cranial nerves innervating the facial muscles
- frequent nasal regurgitation of fluids and difficulty chewing and swallowing from cranial nerve involvement
- drooping eyelids from weakness of facial and extra ocular muscles
- weakened neck muscles that may become too weak to support the head without bobbing, causing the patient to tilt her head back to be able to see . weakened respiratory muscles, decreased tidal volume and vital capacity from impaired transmission to the diaphragm making breathing difficult and predisposing the patient to pneumonia and other respiratory tract infections
- respiratory muscle weakness that’s possibly severe enough to require an emergency airway and mechanical ventilation.
Complications of myasthenia gravis may include:
- respiratory distress
Diagnosis information
Tests to help diagnose myasthenia gravis include:
Neuroanatomy Of Pelvic Floor
The striated muscle forming the urethral rhabdosphincter and the periurethral striated muscle together make up the external urethral sphincter mechanism in humans. In women, the rhabdosphincter forms a 1.5-cm long circular ring around the middle third of the urethra, extending cranially as far as the posterior bladder base. In men, the rhabdosphincter has 3 sections extending over a greater length of urethra. On cystoscopy, this striated muscle can be seen to contract with electrical stimulation of the pudendal nerve.
Spinal cord nuclei supplying the vesicourethral smooth muscle and rhabdosphincter are in the lumbosacral region. The sympathetic autonomic nucleus is in the anteromediolateral gray matter at T10-T12, and the parasympathetic nucleus is at S2-S4. Motor neurons of the urethral rhabdosphincter are in the nucleus of Onufrowicz in the sacral ventral horns. The neurons are smaller, more spherical, and more closely packed than other anterior horn cells.
The nucleus of Onuf and the sacral parasympathetic nucleus are at slightly different levels. This can be of clinical significance in lesions of the conus. The neurons of the Onuf nucleus are relatively spared in many neuromuscular disorders.
Also Check: What Not To Eat With A Urinary Tract Infection
What Are The Classic Patterns Of Weakness Seen In Patients With Mg
The disease is divided into ocular and generalized forms. Both forms can present similarly with extraocular, facial, and oropharyngeal muscles presenting early in the course of the disease. Weakness of these muscles is seen clinically as diplopia, ptosis, dysphagia, and hypophonia, respectively. The ocular form is restricted to these muscles, whereas the generalized form may present initially with, and/or progress to, weakness of flexors and extensors of the neck and proximal muscles of the trunk.
Surgery And Procedures For Stress Incontinence
Sling procedures
Sling procedures involve making an incision in your lower abdomen and inserting a sling around the neck of the bladder to support it. The sling could be made of:
- a synthetic material
- tissue taken from another part of your body
- tissue donated from another person
- tissue taken from an animal , such as cow or pig tissue
Autologous fascial slings are a long-term treatment for stress incontinence and may be the most effective.
Synthetic slings may carry long-term risks of causing difficulty urinating or urge incontinence.
Urethral bulking agents
A urethral bulking agent is a substance that is injected into the walls of your urethra . This increases the size of the urethral walls and allows the urethra to stay closed with more force. A number of different bulking agents are available and there is no evidence that one is more beneficial than another.
This is less invasive than other surgical treatments as it does not require any incisions. However, it is less effective than the other options. The effectiveness of the bulking agents will reduce with time and you may need repeated injections.
Colposuspension
Colposuspension involves making an incision in your lower abdomen and lifting up the neck of your bladder. Stitches through the walls of the bladder neck hold it in place.
There are two types of colposuspension:
Tape procedures for women
Artificial urinary sphincter for men
This treatment is rarely used in women.
Recommended Reading: Kidney Stone In Urinary Tract
The Mg Patient In Crisis
The two primary pharmacological therapies to treat MG crisis are ivIG, at a dose of 0.4 g/kg/day for 5 days or PEusually 46 exchanges . They are equally effective in the treatment of MG crisis or a significant MG relapse . We commonly prescribe ivIG first, unless there are contraindications, and resort to PE as second-line therapy if the patient fails to respond to ivIG. However, if PE is readily available we would recommend using as first-line in the context of MG crisis since it is more rapid in its effect than ivIG. This has been our experience and also previously shown by Qureshi et al. . PE is not without risk however. It is more invasive, more labor-intensive and more expensive than ivIG . PE should be performed via peripheral venous access, where feasible, but central catheters may be necessary in some which pose additional risks of an infection source if mishandled or if left in situ for too long . The same dose of ivIG could be administered over a shorter period for example 23 days if tolerated by the patient. We prefer to administer over 5 days, especially in patients who are ivIG naïve at least initially, and we consider administering over 23 days in subsequent treatments.
How Is Mg Diagnosed
MG is hard to diagnose because weakness is a common symptom of many disorders.
Your doctor will ask you about your symptoms, take a medical history, and perform a physical exam. If your doctor thinks you may have MG, she or he may run some tests:
It is important for you to see a neurologist who is an expert in diagnosing MG. Diagnosis can take a long time , so try to be patient with your doctor.
Read Also: Common Urinary Tract Infection Antibiotics
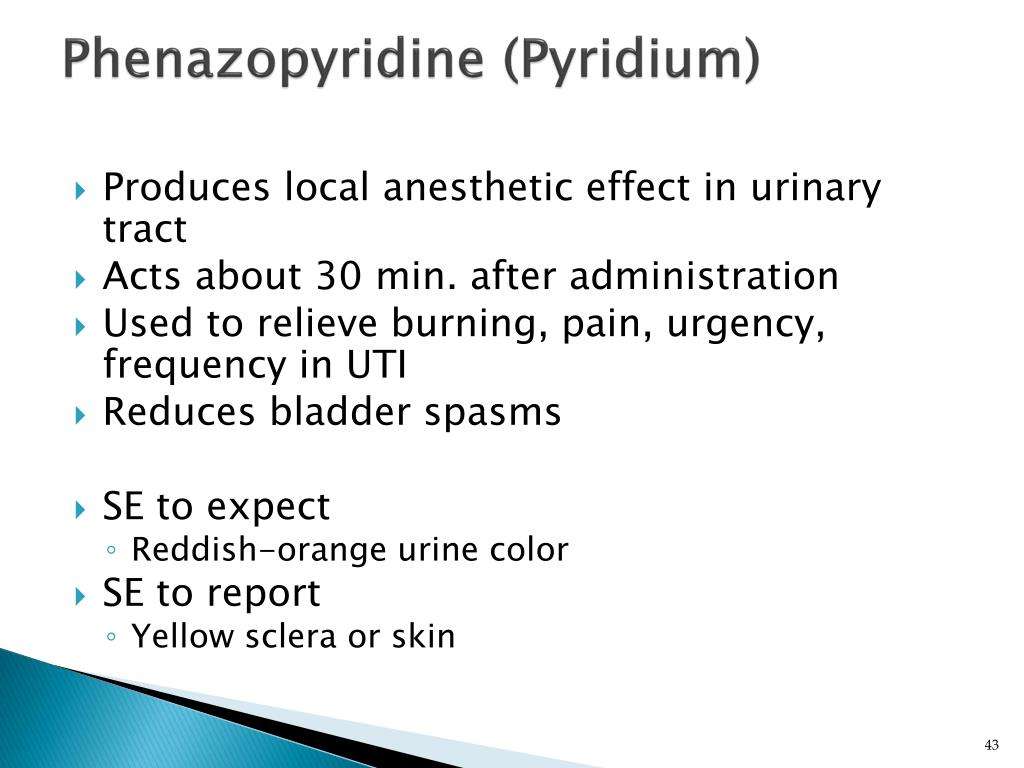
Too Much Pyridostigmine May Increase Overactive Bladder Issues
In certain neurological disorders, lower urinary tract dysfunction is common and has a considerable impact on quality of life. LUTD can be caused by an overactive bladder, which increases the need and urgency to urinate, and may be accompanied by urinary incontinence or loss of bladder control.
Underactive bladder, another form of LUTD, results in a need to wait for the urine flow to start, a need to strain to urinate, or a feeling of being unable to completely empty the bladder. Although a few case reports have described bladder problems in MG patients, little is known about how MG impacts bladder function.
Researchers in Istanbul, Turkey, evaluated the bladder function of 36 patients being treated at their clinic and 29 healthy controls using questionnaires and non-invasive tools, including uroflowmetry and ultrasound imaging.
MG patients , as well as gender- and age-matched controls were asked to complete a three-day urinary voiding diary and respond to two surveys.
Patients mean age was 54, and their mean disease duration was 54 months or about 4.5 years. Most, 19 or 53%, had LOMG, while 17 had EOMG.
The overactive bladder symptom score was used to evaluate related symptoms, and the international consultation on incontinence-short form to assess urinary incontinence. In both tests, higher scores indicated more severe symptoms.
Investigators also found that disease duration and the duration of urinary symptoms were greater in patients who did not have ACh-Ab antibodies.
What Research Is Being Done
The National Institute of Neurological Disorders and Stroke, within the National Institutes of Health, conducts and supports research on MG. Research findings have led to more timely and accurate diagnoses. New and enhanced therapies have improved management of the disorder.
Despite these advances, there is still much to learn. The ultimate goal of MG research is to increase understanding of the disorder. Researchers are seeking to learn what causes the autoimmune response in MG and to better define the relationship between the thymus gland and MG.
Don’t Miss: Why Am I Prone To Urinary Tract Infections
Fda Approves New Treatment For Myasthenia Gravis
SILVER SPRING, Md., Dec. 17, 2021 /PRNewswire/ — The U.S. Food and Drug Administration today approved Vyvgart for the treatment of generalized myasthenia gravis in adults who test positive for the anti-acetylcholine receptor antibody.
Myasthenia gravis is a chronic autoimmune, neuromuscular disease that causes weakness in the skeletal muscles that worsens after periods of activity and improves after periods of rest. Myasthenia gravis affects voluntary muscles, especially those that are responsible for controlling the eyes, face, mouth, throat, and limbs. In myasthenia gravis, the immune system produces AChR antibodies that interfere with communication between nerves and muscles, resulting in weakness. Severe attacks of weakness can cause breathing and swallowing problems that can be life-threatening.
“There are significant unmet medical needs for people living with myasthenia gravis, as with many other rare diseases,” said Billy Dunn, M.D., director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research. “Today’s approval is an important step in providing a novel therapy option for patients and underscores the agency’s commitment to help make new treatment options available for people living with rare diseases.”
Story continues below video
The FDA granted this application Fast Track and Orphan Drug designations. The FDA granted the approval of Vyvgart to argenx BV.
# # #
Media Contact: , 202-281-5237 Consumer Inquiries: or 888-INFO-FDA
What Is Myasthenia Gravis
MG is an autoimmune disorder affecting the neuromuscular junction characterized by a T-cellmediated response targeting the postsynaptic acetylcholine receptor or receptor-associated proteins. Patients typically have the classic pattern of fatigable weakness, where repetitive stimulation of a muscle results in progressive weakness.
Don’t Miss: How Does A Urinary Tract Infection Feel
The Lymphatic System And Immune Response Marieb Does Alcohol Bring Your Immune System Down
Immune System Packet Answers Immune System Web Answer Key. Hormones That Depress Immune System Stress What Happens When You Overload Your Immune System Immune System In Bloodstream. Immune System Vs Yellow Fever How Does Myasthenia Gravis Affect The Immune System, Spleen Related To Immune System Rabbit Versus Mouse Immune System.
| how does the immune system respond to diabetes | 7mo immune system |
|---|
How Ms Affects Your Bladder
Over time, about 80% of MS patients will experience bladder problems. An overactive bladder is common, where the nerve damage results in frequent, uncontrollable urges to empty, even though the bladder isn’t full.
Problems emptying the bladder completely are also very common. The muscles in the pelvic floor and the sphincter muscle around the urethra contract spontaneously during emptying. This closes the urethra, resulting in the bladder not being properly emptied. The residual urine then leads to the feeling of needing to urinate again, leading to more bathroom trips than if the bladder had been completely emptied.
The progression of MS can swing wildly urinating will be more problematic in some periods, relatively easy in others. It is still very important to treat bladder emptying problems consistently. Residual urine can lead to urinary tract infections, which in turn can cause new attacks or the return of an attack that had previously receded.
You can also find additional information in our enCATHopedia leaflet.
Read Also: E Coli In Urinary Tract
What Are The Signs And Symptoms Of Mg
MG can affect any muscle, but the muscles that control eye and eyelid movement, facial expression, and swallowing are most often affected. In some people, the first symptom is weakness of the eye muscles. In others, having a hard time swallowing, talking, and breathing can be the first signs. Different people have different levels of muscle weakness. Symptoms may include:
- Drooping of one or both eyelids
- Blurred or double vision
- Having a hard time swallowing
- Trouble talking
- Shortness of breath
The onset of the disorder may be sudden. And the symptoms often are not immediately recognized as MG.
Some drugs can trigger or worsen MG symptoms.
The Refractory Mg Patient And Novel Therapies
In our experience, where we have treated a small cohort of 17 MG patients with MuSK-MG, AChR-MG, and MG with no detectable antibodies, the majority of patients improved significantly but remain dependent on immunosuppression . Our single MuSK-MG patient, within this small cohort, responded best to Rituximab although this did not induce complete remission of her disease. In contrast, about a third of MG patients did not respond to Rituximab and their MG status was not altered by this therapy. In general, we have found that the drug is well-tolerated with minimal side effects. However, in two patients we have observed delayed neutropenia developing many months after Rituximab treatment, including one patient whose presentation was complicated by two neutropenic sepsis episodes several months after their Rituximab treatment. This has been observed in other patient groups treated with Rituximab .
Efgartigimod has been trialed in generalized MG in a phase-2 randomized double-blind, placebo-controlled study in 15 centers . ARGX-113 is the anti-neonatal Fc receptor immunoglobulin IgG1 fragment. It has been modified to increase its normal affinity for IgGs, thus blocking the formation of disease-causing IgG. Efgartigimod was well-tolerated in this trial. In the 12 patients treated with the active drug, there was a rapid decline in total Ig levels and in AChR titers, which in turn correlated with a clinical improvement of their MG, and this was sustained in the majority.
Read Also: How To Reverse Urinary Retention
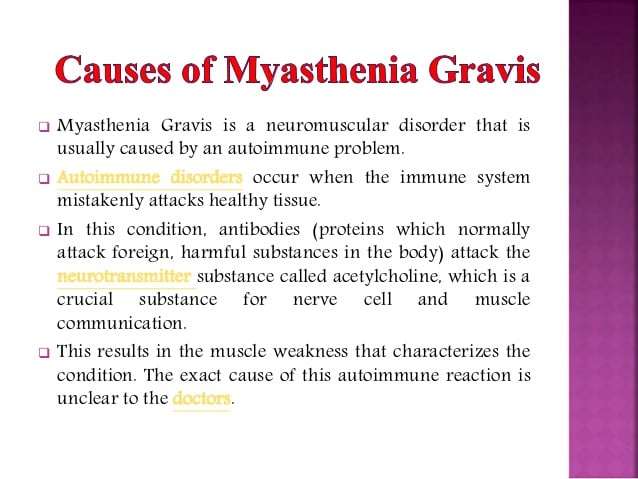
What Causes Myasthenia Gravis
Myasthenia gravis is not inherited and it is not contagious. It generally develops later in life when antibodies in the body attack normal receptors on muscle. This blocks a chemical needed to stimulate muscle contraction.
A temporary form of myasthenia gravis may develop in the fetus when a woman with myasthenia gravis passes the antibodies to the fetus. Generally, it resolves in 2 to 3 months.
Medication For Urge Incontinence And Overactive Bladder Syndrome
If bladder training is not an effective treatment for your urge incontinence, your doctor may prescribe an antimuscarinic. Antimuscarinics may also be prescribed if you have overactive bladder syndrome , which is the frequent urge to urinate with or without urinary incontinence.
The first antimuscarinic that may be tried is called oxybutynin. There are two different types of oxybutynin tablets, and it is also available as a patch that you stick to your skin. If oxybutynin is not effective or unsuitable, other antimuscarinics that may be prescribed include:
- darifenacin
- tolterodine
- trospium
Your doctor will usually start you at a low dose to minimise any possible side effects. The dose can then be increased until the medicine is effective.
You will be assessed after six weeks to see how you are getting on with the medication, and again after three to six months to see if you still need it.
Antimuscarinics should not be taken or should be used with caution by:
- people with an untreated eye condition called angle closure glaucoma
- people with myasthenia gravis, a condition that causes some muscles around your body to become weak
- people with severe ulcerative colitis, a long-term condition that affects the colon
Your doctor will discuss any other medical conditions you have to determine which antimuscarinics are suitable for you.
Side effects
There are many possible side effects of antimuscarinics, including:
- dry mouth
For more information see our .
Read Also: Symptoms Of Pinworms In Urinary Tract
How Is Myasthenia Gravis Diagnosed
Your doctor can diagnose myasthenia gravis based on your symptoms and certain tests. During the physical exam, your doctor will ask about your medical history and symptoms.
A common way to diagnose myasthenia gravis is to test how you respond to certain medicines. Muscle weakness often dramatically improves for a brief time when you are given an anticholinesterase medicine. If you respond to the medicine, it confirms myasthenia gravis.
Other tests that may be done include:
-
Blood tests. These tests look for antibodies that may be present in people with myasthenia gravis.
-
Genetic tests. These tests are done to check for conditions that run in families.
-
Nerve conduction studies. A test called repetitive nerve stimulation is used to diagnose myasthenia gravis.
-
Electromyogram . A test that measures the electrical activity of a muscle. An EMG can detect abnormal electrical muscle activity due to diseases and neuromuscular conditions.