What Is Urinary Incontinence
Many people experience involuntary leakage of urine from the bladder. This condition is called urinary incontinence. It affects nearly a quarter to a third of men and women in the United States. That is millions of Americans.
Urinary incontinence is the leaking of urine from the bladder that you cant control. There are different kinds of urinary incontinence, and not all types are permanent. An experienced doctor can help you find the best treatment for your urinary incontinence.
Stress urinary incontinence is when the muscles arent strong enough to hold urine in the body. SUI shows itself through physical symptoms, including involuntary leaking of urine through the bladder when active.
Overactive bladder is a strong sudden urge to urinate, which may or may not cause urine to leak from the bladder.
In some cases, people experience a combination of both SUI and OAB. This shows itself through physical symptoms. If this is the case for you, you will find involuntary leaking of urine through the bladder and strong sudden urges to urinate that you cant control.
Overflow incontinence is when the bladder isnt able to empty itself completely. Overflow incontinence shows itself through physical symptoms, including constant dribbling of small amounts of urine when the bladder is full.
These symptoms are not just physical. Urinary incontinence has emotional and psychological effects, too.
Recommended Reading: Does Azo Urinary Pain Relief Work
Pelvic Floor Muscle Training
Your pelvic floor muscles surround the bladder and urethra and control the flow of urine as you pee.
Weak or damaged pelvic floor muscles can cause urinary incontinence, so exercising these muscles is often recommended.
A GP may refer you to a specialist to start a programme of pelvic floor muscle training.
The specialist will assess whether you’re able to squeeze your pelvic floor muscles and by how much.
If you can contract your pelvic floor muscles, you’ll be given an exercise programme based on your assessment.
Your programme should include a minimum of 8 muscle contractions at least 3 times a day and last for at least 3 months. If the exercises are helping after this time, you can keep on doing them.
Research has shown that pelvic floor muscle training can benefit everyone with urinary incontinence.
Find out more about pelvic floor exercises.
What If I Miss A Dose
If you miss a dose of Gemtesa, take it as soon as you remember. However, if its almost time for your next dose, you may need to skip the missed dose and take your next dose at the scheduled time.
If you have any questions about when to take your next dose of Gemtesa after you miss a dose, talk with your doctor or pharmacist.
To help make sure that you dont miss a dose, try using a medication reminder. This can include setting an alarm or timer on your phone or downloading a reminder app. A kitchen timer can work, too.
You May Like: Cvs Urinary And Prostate Plus
Behavioral Therapies For Oab
Some people with urinary incontinence may get relief by making simple changes to their lives and that’s what experts recommend trying first.
If you have stress incontinence, for instance, in which you leak urine when you cough, sneeze, or laugh, your doctor may tell you to limit how much you drink.
If you have urge incontinence, in which you get the sudden urge to urinate and can’t always make it to the bathroom in time, your doctor may tell you to avoid spicy foods, caffeine, and carbonated drinks, because they can irritate the bladder and make the problem worse.
Exercises to strengthen the pelvic floor muscles, known as Kegels, can help people with stress incontinence. Kegels can also help people with urge incontinence. Sometimes, Kegels are combined with biofeedback techniques to help you know if you are doing the exercises properly.
For urge incontinence, bladder training, sometimes called bladder retraining, can also help. This involves gradually increasing the interval time between trips to the bathroom, working up to longer and longer intervals between bathroom stops.
Guidance For Industry And Fda Staffclinical Investigations Of Devices Indicated For The Treatment Of Urinary Incontinence
This guidance represents the Food and Drug Administrations current thinking on this topic. It does not create or confer any rights for or on any person and does not operate to bind FDA or the public. You can use an alternative approach if the approach satisfies the requirements of the applicable statutes and regulations. If you want to discuss an alternative approach, contact the FDA staff responsible for implementing this guidance. If you cannot identify the appropriate FDA staff, call the appropriate number listed on the title page of this guidance.
You May Like: Fastest Way To Cure Urinary Tract Infection
Using Artificial Intelligence In Treating Overactive Bladder
Overactive bladder is a chronic condition for which roughly 70 percent of cases are idiopathic, Dr. Sheyn says. Furthermore, many patients suffer for up to seven years from onset of symptoms until they start appropriate treatment. Behavior modification and pelvic floor physical therapy are first-line therapies before advancing to bladder training and more invasive treatments.
Renalis, a digital therapeutics company, has developed an Artificial Intelligence-based platform to help patients manage OAB.
Renalis helps people keep track of pelvic floor therapy and fluid intake and make adjustments as needed, Dr. Sheyn says. It includes an educational component and, in some cases, can replace physical therapy. You dont really realize how OAB can affect your quality of life until it becomes a problem. Renalis helps increase awareness of, and attention to, OAB.
Dr. Sheyn will conduct a pilot study in 30 to 50 patients who are treatment naive or who have never been treated for OAB by a urogynecologist or a urologist. Participants will download the app and use it in a real-world setting, with the hopes it significantly improves their symptoms.
Dr. Hijaz says UH is excited about the study and the ability to have a chatbot as a therapeutic option to help patients navigate OAB in a non-intrusive way. Through one-to-one interactions, the chatbot can analyze symptoms and guide patients through therapy.
Meet The Expert: Dr David Beatty Md
Dr. David Beatty has been a doctor for over 30 years in England. A large part of this role has been around helping people make lifestyle changes. Recommending and educating people on healthy habits such as sleep, nutrition and weight loss has been crucial to his career.
Dr. Beatty has been featured in Healthline, Best Life Online, Up Journey, and much more. You can learn more about David and his qualifications here.
In fact, pregnancy and vaginal delivery are often responsible. Uterine or vaginal wall prolapse can also play a part.
If youre tired of wearing bulky pads or maybe even incontinence briefs, the best urinary incontinence treatments can help you regain your freedom.
Ill walk you through the 10 best urinary incontinence treatments. From convenient, non-invasive shorts to innovative pelvic floor exercisers, consider this your judgment-free guide to a leak-free life.
You May Like: Menopause Urinary Tract Infection Symptoms
Urinary Incontinence In Older Adults
Urinary incontinence means a person leaks urine by accident. While it can happen to anyone, urinary incontinence, also known as overactive bladder, is more common in older people, especially women. Bladder control issues can be embarrassing and cause people to avoid their normal activities. But incontinence can often be stopped or controlled.
What happens in the body to cause bladder control problems? Located in the lower abdomen, the bladder is a hollow organ that is part of the urinary system, which also includes the kidneys, ureters, and urethra. During urination, muscles in the bladder tighten to move urine into the tube-shaped urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder dont work the way they should, urine can leak, resulting in urinary incontinence.
Incontinence can happen for many reasons, including urinary tract infections, vaginal infection or irritation, or constipation. Some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
- Weak bladder or pelvic floor muscles
- Overactive bladder muscles
- Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinsons disease
- Diseases such as arthritis that may make it difficult to get to the bathroom in time
Most incontinence in men is related to the prostate gland. Male incontinence may be caused by:
Who Needs Urinary Incontinence Treatment
Your pelvic floor muscles are responsible for much more than just keeping your bathroom breaks in check. These muscles can also increase feelings of pleasure, heighten mens staminaand performance, and reduce pain.
Some people dont tolerate minor degrees of incontinence. Others will put up with almost total urinary incontinence and still not seek medical help, Dr. Beatty said.
Overall, its advisable to have treatment, on medical grounds, if there is significant urine retention. If the bladder overfills the urine can back up into the kidneys and this can impair kidney function and cause renal failure.
So the best urinary incontinence treatments are for you if you frequently or occasionally experience bladder leaks when exercising, sneezing, or laughing.
If you have trouble making it to the bathroom, using one of the options listed here could be very beneficial.
Also Check: What Causes Urinary Retention In Males
Transvaginal Needle Suspension Procedures
Advantages to the transvaginal approach include the avoidance of a large, transfascial abdominal incision shorter operative times less postoperative discomfort shorter hospital stay and the ability to repair coexisting vaginal pathology through the same or slightly extended incision. Disadvantages include a potentially lower long-term cure rate poor intraoperative visualization risk of injury to the bladder and urethra during blind passage of the needles through the retropubic space risk of significant bleeding in the retropubic space with poor operative access from the vaginal incisions and, lastly, infection or erosion of a foreign body if suture buttresses are utilized .
Basic Evaluation Of Stress Urinary Incontinence
When women are evaluated for SUI, counseling about treatment should begin with conservative options. The minimum evaluation before primary midurethral sling surgery in women with symptoms of SUI includes the following six steps: 1) history, 2) urinalysis, 3) physical examination, 4) demonstration of stress incontinence, 5) assessment of urethral mobility, and 6) measurement of postvoid residual urine volume.
Also Check: What Is A Natural Cure For Urinary Tract Infection
Treating And Managing Urinary Incontinence
Today, there are more treatments and ways to manage urinary incontinence than ever before. The choice of treatment depends on the type of bladder control problem you have, how serious it is, and what best fits your lifestyle. As a general rule, the simplest and safest treatments should be tried first.
A combination of treatments may help you get better control of your bladder. Your doctor may suggest you try the following:
Do Pelvic Floor Muscle Exercises
Strong pelvic floor muscles hold in urine better than weak muscles. You can strengthen your pelvic floor muscles by doing Kegel exercises. These exercises involve tightening and relaxing the muscles that control urine flow. Researchers found that women who received pelvic floor muscle training had fewer leaks per day than women who didnt receive training.6 You should not do pelvic floor exercises while youre urinating.
Men can also benefit from pelvic floor muscle exercises. Strengthening these muscles may help a man leak urine less often, especially dribbling after urination.
A health care professional, such as a physical therapist trained in pelvic floor therapy, can help you get the most out of your Kegel exercises by helping you improve your core muscle strength. Your core includes your torso muscles, especially the lower back, pelvic floor muscles, and abdomen. These muscles keep your pelvis lined up with your spine, which helps with good posture and balance. Your physical therapist can show you how to do some exercises during daily activities, such as riding in a car or sitting at a desk.
You dont need special equipment for Kegel exercises. However, if you are unsure whether you are doing the exercises correctly, you can learn how to perform Kegel exercises properly by using biofeedback, electrical stimulation, or both. Biofeedback uses special sensors to measure muscle contractions that control urination.
You May Like: Azo Urinary Pain Relief For Males
Medications For Urinary Incontinence
Other names: Bladder, Weak Incontinence Incontinence, Urge Urge Incontinence Weak Bladder
Incontinence is the inability to control the passage of urine. This can range from an occasional leakage of urine, to a complete inability to hold any urine.
The three main types of urinary incontinence are:
Stress incontinence — occurs during certain activities like coughing, sneezing, laughing, or exercise.
Stress incontinence is a bladder storage problem in which the strength of the muscles that help control urination is reduced. The sphincter is not able to prevent urine flow when there is increased pressure from the abdomen.
Stress incontinence may occur as a result of weakened pelvic muscles that support the bladder and urethra or because of a malfunction of the urethral sphincter.
Treatment for stress incontinence may include behavioral changes, medication, pelvic floor muscle training or surgery.
Urge incontinence — involves a strong, sudden need to urinate followed by instant bladder contraction and involuntary loss of urine. You don’t have enough time between when you recognize the need to urinate and when you actually do urinate.
In most cases of urge incontinence, no specific cause can be identified.Although urge incontinence may occur in anyone at any age, it is more common in women and the elderly.
Treatment for urge incontinence may include medication, retraining, and surgery.
Mixed incontinence — contains components of both stress and urge incontinence.
Implications For Patient Care
Its a minimally invasive procedure that only requires local anesthesia and normally takes less than 15 minutes, explains Dr. Goldman. If the study validates its use, it could be a game-changer in the treatment of SUI, allowing a truly minimally invasive treatment utilizing no foreign material but only the patients own cells.
Cleveland Clinic will begin enrolling patients later this year.
You May Like: Does Azo Urinary Pain Relief Get Rid Of Uti
New Relief For Stress Incontinence
‘Tension-Free’ Relief
Women who suffer from stress urinary incontinence worry about coughing, sneezing, even laughing in public for fear of having an accident. For some the fear of embarrassment is so great that they become virtual recluses, staying at home and avoiding any social contact.
Even with this anxiety, however, 62% of women sufferers wait a year or longer before discussing the condition with their doctor, reports a new Multi-sponsor Surveys’ Gallup Study of women with SUI.
“It’s usually when something really embarrassing happens to them in public that they finally seek help,” says Jill Peters-Gee, MD, director of the Continence Care Program for Women’s Health Connecticut. Most women cope with SUI by wearing pads, says Peters-Gee, because they don’t know that SUI can now be easily treated with a simple surgical procedure.
First though, a definition. SUI is the involuntary loss of urine due to any physical activity that puts strain on the bladder, says Peters-Gee. The most common type of incontinence, SUI affects nearly 8 million women in the U.S, and occurs when the pelvic muscles supporting the bladder and urethra have been damaged or weakened. Some of the physical changes that can lead to SUI include childbirth, pelvic or gynecologic surgery, menopause or estrogen deficiency, obesity, and chronic constipation
Up to 80% of cases of female incontinence are treatable, says Peters-Gee, with treatment options including:
Show Sources
Vibegrons Mechanism Of Action
Vibegron is a small molecule, selective human beta-3 adrenergic agonist that binds to and activates the beta-3 adrenergic receptor on the bladder.
Activation of the beta-3 adrenergic receptor increases the capacity of the bladder by calming the detrusor smooth muscle during the bladder filling.
The drugs safety and efficacy in children remain unestablished.
You May Like: Meds For Urinary Tract Infection Over The Counter
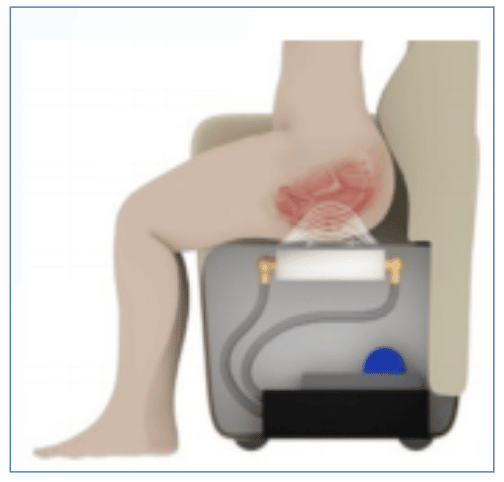
Posterior Tibial Nerve Stimulation
Posterior tibial nerve stimulation involves the use of electrical impulses and is a form of neuromodulation employed to improve urinary symptoms37. This can be in the form of percutaneous tibial nerve stimulation , which uses a needle, and transcutaneous tibial nerve stimulation , which uses pads. This treatment usually involves weekly 30-minute visits to the hospital for up to 12 weeks. More recently, implantable devices have become available.
The RENOVA iStim is a wirelessly powered implant. The implant is surgically inserted under local anaesthesia. The incision is made 3 cm superior and 2 cm posterior to the medial malleolus. The electrode is placed near the tibial nerve and secured with a non-absorbable suture. An external control unit is worn around the ankle to activate the electrodes. This unit is worn six times a week for 30 minutes to activate treatment37,38. A study of 15 patients showed a significant improvement in frequency, urgency, and urgency incontinence episodes at 3 months38. There was also significant improvement in quality of life. Three patients required a week of antibiotics and three required a week of analgesics. One device was explanted for suspected infection, although cultures were negative. None of the patients reported difficulty in operating the device.
When To See A Health Care Provider And What To Expect
Talk to your health care provider if you have urinary incontinence or any signs of a bladder problem, such as:
- Needing to urinate more frequently or suddenly
- Urinating eight or more times in one day
- Passing only small amounts of urine after strong urges to urinate
- Trouble starting or having a weak stream while urinating
Your doctor may recommend urodynamic testing and perform the following to try to figure out what might be causing your bladder problem:
- Give you a physical exam and take your medical history.
- Ask about your symptoms and the medications you take.
- Take urine and blood samples.
- Examine the inside of your bladder using a cystoscope a long, thin tube that slides up into the bladder through the urethra. This is usually done by a urinary specialist.
- Fill the bladder with warm fluid and use a cystoscope to check how much fluid your bladder can hold before leaking.
- Order or perform a bladder ultrasound to see if you are fully emptying your bladder with each void.
- Ask you to keep a daily diary of when you urinate and when you leak urine. Your primary care doctor may also send you to a urologist, a doctor who specializes in urinary tract problems.
Recommended Reading: I Have A Urinary Tract Infection